DermNet provides Google Translate, a free machine translation service. Note that this may not provide an exact translation in all languages
Home Dermoscopy Other algorithms for melanocytic lesions CME
Dermoscopy
Other algorithms for melanocytic lesions
Created 2008.
Learning objectives
- Describe several algorithms for evaluating melanocytic lesions by dermoscopy
Introduction
The first step algorithm identifies whether a lesion is melanocytic or nonmelanocytic. Various algorithms may be used to distinguish benign melanocytic lesions from malignant melanoma.
If these algorithms appear too complicated, use the 3-point checklist to identify malignant pigmented lesions.
ABCD rule
The ABCD rule (Stolz method) is used for the dermatoscopic differentiation between benign melanocytic lesions and melanoma. The likelihood of melanoma depends on adding up the scores for different features as shown below.
| Criteria | Score X | Factor = | Results |
|---|---|---|---|
| Asymmetry In perpendicular axes: contour, colours and structures |
0–2 | 1.3 | 0–2.6 |
| Borders 8 segments: abrupt ending of pigment pattern |
0–8 | 0.1 | 0–0.8 |
| Colours White, red, light-brown (tan), dark-brown, blue-grey, black |
1–6 | 0.5 | 0.5–3.0 |
| Differential structural components or dermatoscopic structures (pigment network, structureless areas, dots, aggregated globules, branched streaks) | 1–5 | 0.5 | 0.5–2.5 |
| Total score | |||
| Benign | < 4.76 | ||
| Suspicious | > 4.76–5.45 | ||
| Melanoma | > 5.45 | ||
Blum's modified ‘ABC-point list’ is simpler to use:
A – asymmetry of outer shape or differential structures inside the lesion in at least 1 axis
B – the abrupt cutoff of the network at the border in at least one-quarter of the circumference
C – 3 or more colours
D – 3 or more differential structures
E – noticed a change (evolution) in the last 3 months
Menzies method
Menzies method to distinguish the dermatoscopic features of benign melanocytic lesions from melanoma.
Negative features (benign lesions):
- Symmetrical pattern (colours, structure)
- Single colour
Positive features (melanoma):
- Blue-white veil
- Multiple brown dots
- Pseudopods
- Radial streaming
- Scar-like depigmentation
- Multiple (5-6) colours
- Multiple blue/grey dots
- Broadened network
Seven-point rule
7-point checklist (Argenziano) for the dermoscopic differentiation between benign melanocytic lesions and melanoma (scores in brackets). The scores should be added up. Three or more indicates melanoma.
- Atypical pigment network (2)
- Blue-whitish veil (2)
- Atypical vascular pattern (2)
- Irregular streaks (1)
- Irregular dots/globules (1)
- Irregular blotches (1)
- Regression structures (1)
The seven-point rule has been revised (2011) so that each item scores 1 (total is 7). IN patients with atypical naevi, any lesion with a score of one should be carefully examined and excision of such lesions will pick up many early-stage melanomas.
C.A.S.H. acronym
C.A.S.H. (Kopf et al) is used for the dermatoscopic differentiation between benign melanocytic lesions and melanoma (scores in brackets).
| Low | Medium | High | |
|---|---|---|---|
| Colours: few vs many Light brown, dark brown, black, red, white, blue Score 1 point for each colour |
1-2 colours (1-2 points) | 3-4 colours (3-4 points) | 5-6 colours (5-6 points) |
| Architecture: order vs disorder Score 0-2 points |
None or mild disorder (no points) | Moderate disorder (1 point) | Marked disorder (2 points) |
| Symmetry vs asymmetry Consider contour, colours and structures Score 0-2 points |
Symmetry in 2 axes (no points) | Symmetry in 1 axis (1 point) | No symmetry (2 points) |
| Homogeneity vs Heterogeneity Consider pigment network, dots/globules, blotches, regression, streaks, blue-white veil, polymorphous vessels Score 1 point for each structure |
Only one structure (1 point) | 2 types of structure (2 points) | 3 or more structures (3-7 points) |
Add up the scores for a total C.A.S.H. score (2 to 17).
- C.A.S.H. score of 7 or less is likely benign.
- C.A.S.H. score of 8 or more is suspicious of melanoma.
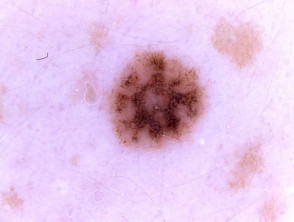
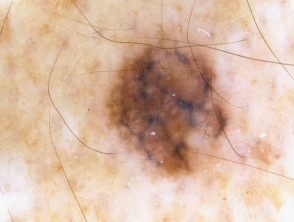
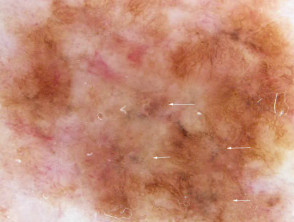
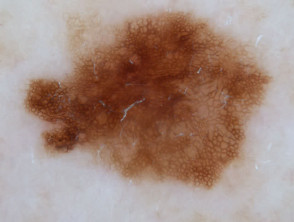
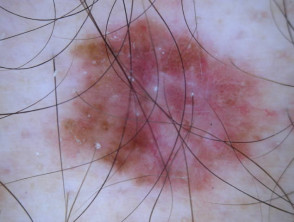
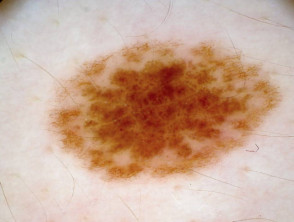
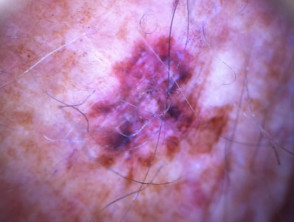
C.A.S.H. in melanoma
CHAOS and clues
A modified form of pattern analysis (Kittler, Rosendahl et al) looks for CHAOS (asymmetry of structure and/or colour) and at least one clue to diagnose malignancy. It can be applied to melanocytic and nonmelanocytic lesions. This method does not use the 2-step rule.
Patterns are described by multiple elements of the same type: lines, dots, clods, circles, pseudopods (a line with a bulbous end) and structureless areas. Structureless areas are made up of colours: black, dark brown, light brown, grey, blue, orange, yellow, white, red and purple.
- A single pattern or a single colour is a symmetrical structure and is benign.
- Two patterns can have one pattern inside the other pattern or the two patterns may be regularly distributed. Such lesions have a symmetrical structure. Two patterns can be distributed asymmetrically.
- Multiple patterns/colours may result in symmetrical structure if forming concentric zones. Otherwise, they result in an asymmetrical structure.
Symmetry of structure
Asymmetrical patterns should lead to looking for specific clues to malignancy. The clues to malignancy (melanoma and nonmelanocytic tumours) are:
- Thick reticular lines
- Grey or blue structures of any kind
- Pseudopods or radial lines at the periphery
- Black dots in the periphery
- Eccentric structureless area of any colour
- Polymorphous vascular pattern
- White lines
- Parallel lines on ridges
- Large polygons.
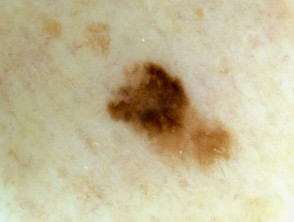
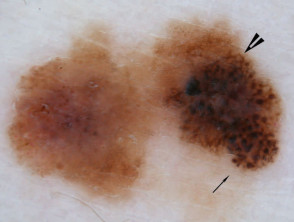
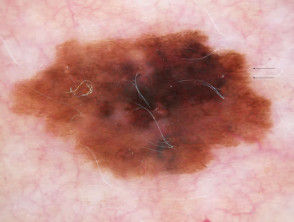
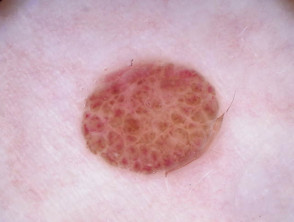
Chaos + eccentric structureless area, blue/grey structures, white lines, peripheral black dots Chaos + eccentric structureless area, polygons Chaos + eccentric structureless area, polymorphous vessels Chaos + blue/grey structures, polymorphous vessels Chaos + peripheral black dots, blue/grey structures, eccentric structureless area, white lines, poly Chaos + eccentric structureless area, peripheral black dots, polygons Chaos + thickened reticular network, eccentric structureless area Chaos + thickened reticular network, eccentric structureless area, polygonsCHAOS and clues in melanoma




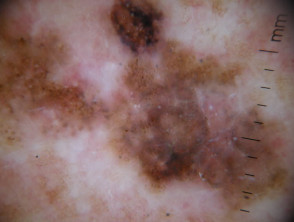
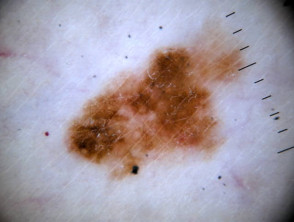

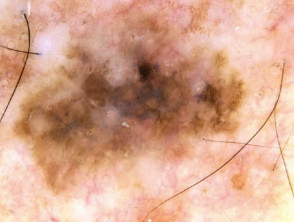
Some of these images are of poor quality, but the algorithm still works.
The BLINK algorithm
The BLINK algorithm has been devised to identify malignant lesions, particularly nodular melanoma, as this tumour often lacks conventional dermatoscopic features. It can also be used for nonmelanocytic lesions.
| Benign | If not, then consider the following: | |
| Lonely | An ugly duckling | Score 1 |
| Irregular | Asymmetrical pigmentation pattern or > 1 colour | Score 1 |
| Nervous | Nervous patient OR changing lesion | Score 1 |
| Known | Known clues to malignancy | Score 1 |
Clues to malignancy are:
- Atypical network
- Segmental streaks
- Irregular black dots, globules, clods
- Eccentric structureless zone
- Irregular blue or grey in colour
- Polymorphous, arborising, glomerular vessels
- Parallel ridge pattern or diffuse irregular brown/black pigmentation in acral lesion
A score of ≥2 requires a biopsy.
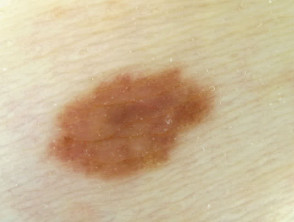
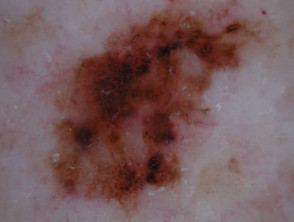
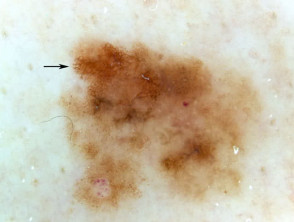
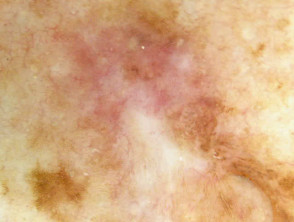
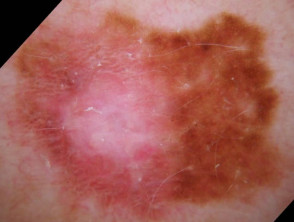
I=1, K=1 (atypical network, eccentric structureless zone) I=1, K=1 (segmental streaks, irregular black dots, eccentric structureless zone) I=1, K=1 (atypical network, irregular black dots, eccentric structureless zone) I=1, K=1 (atypical network, irregular black dots/clods) I=1, K=1 (atypical network, segmental streaks, eccentric structureless zone) I=1, K=1 (atypical network, eccentric structureless zone)BLINK in melanoma
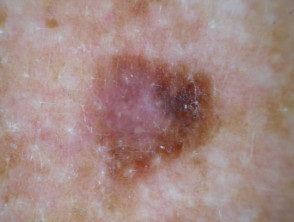

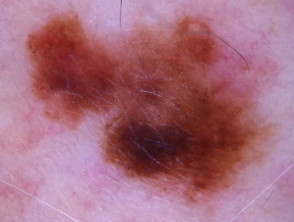


Some of these images are of poor quality, but the algorithm still works.
TADA
TADA is an acronym for Triage Amalgamated Dermoscopic Algorithm. TADA does not require a diagnosis to be made in order to decide if the lesion should be excised or referred to an expert. TADA is reported to have a sensitivity of 94.8% and specificity of 72.3% for malignant skin lesions.
The first step is to determine whether the lesion has features of:
- Angioma
- Dermatofibroma
- Seborrhoeic keratosis.
If yes, exclude from further analysis. If no, is there any architectural disorder? If there is architectural disorder, does the lesion have one or more of the following 6 predictive factors?
- Starburst pattern
- Blue-black or grey structures
- Shiny white structures
- Negative network
- Ulcer/erosion
- Vessels
If yes, consider excision or refer.
If no, the lesion is likely to be benign. Any doubt, follow-up or refer.
Activity
Find the evidence to support the use of the algorithms. Which is the best?
Related information
References
- Dermoscopy of pigmented skin lesions: results of a consensus meeting via the Internet. J Am Acad Dermatol. 2003 May;48(5):679-93. PubMed.
- Chen LL, Dusza SW, Jaimes N, Marghoob AA. Performance of the First Step of the 2-Step Dermoscopy Algorithm. JAMA Dermatol. 2015;151(7):715-721. doi:10.1001/jamadermatol.2014.4642. PubMed.
- Johr RH. Dermoscopy: alternative melanocytic algorithms-the ABCD rule of dermatoscopy, Menzies scoring method, and 7-point checklist. Clin Dermatol. 2002 May-Jun;20(3):240-7. PubMed.
- Dolianitis C, Kelly J, Wolfe R, Simpson P. Comparative performance of 4 dermoscopic algorithms by nonexperts for the diagnosis of melanocytic lesions. Arch Dermatol. 2005 Aug;141(8):1008-14. PubMed.
- Blum A, Rassner G, Garbe C. Modified ABC-point list of dermoscopy: A simplified and highly accurate dermoscopic algorithm for the diagnosis of cutaneous melanocytic lesions. J Am Acad Dermatol. 2003 May;48(5):672-8. PubMed.
- Argenziano G, Catricalà C, Ardigo M, Buccini P, De Simone P, Eibenschutz L, Ferrari A, Mariani G, Silipo V, Sperduti I, Zalaudek I. Seven-point checklist of dermoscopy revisited. Br J Dermatol. 2011 Apr;164(4):785-90. PubMed.
- Henning JS, Dusza SW, Wang SQ; et al. The C.A.S.H. algorithm for dermoscopy. J Am Acad Dermatol. 2007;56(1):45-52. PubMed.
- Algorithm for a specific diagnosis by Harald Kittler, M.D. and Philipp Tschandl, M.D., Derm101.com
- Rogers T, Marino ML, Dusza SW, Bajaj S, Usatine RP, Marchetti MA, Marghoob AA. A Clinical Aid for Detecting Skin Cancer: The Triage Amalgamated Dermoscopic Algorithm (TADA). J Am Board Fam Med. 2016 11/12;29(6):694-701. doi: 10.3122/jabfm.2016.06.160079. PubMed PMID: 28076252. PubMed.
On DermNet NZ
- Dermatoscope overview
- Dermatoscopy quizzes
- Dermatoscopy Information for patients
- Image acquisition
Other websites
Books about skin diseases
See the DermNet NZ bookstore.
Sign up to the newsletter
© 2024 DermNet.
DermNet does not provide an online consultation service. If you have any concerns with your skin or its treatment, see a dermatologist for advice.