DermNet provides Google Translate, a free machine translation service. Note that this may not provide an exact translation in all languages
Home Phototherapy Photosensitivity CME
Phototherapy
Photosensitivity
Created 2007.
Learning objectives
- Recognise photosensitivity and distinguish common variants
- Provide advice about photoprotection
Introduction
The term photosensitivity describes an abnormal response of the skin to light, occurring within minutes to weeks of exposure and lasting for minutes to months.
Photosensitivity may result in phototoxic sunburn-type response or a variety of idiopathic or photoallergic rashes.
Distribution involves areas exposed to the light, predominantly face, neck, V of neck, backs of hands, lower legs and tops of feet. Unaffected areas include:
- Face: under hairline, behind ear, under chin, upper eyelid, furrows and creases
- Hands: under watchstrap and rings, between digits.
Precise diagnosis can be difficult and requires a careful history.
- Skin biopsy may be helpful in persistent eruptions
- Arrange appropriate blood tests for suspected connective tissue disease or porphyria
- Patch testing and photopatch testing are helpful if the morphology is a dermatitis
- Rarely, broadband or monochromator phototesting is helpful to identify responsible wavelengths. Monochromator testing is not available in New Zealand (2005).
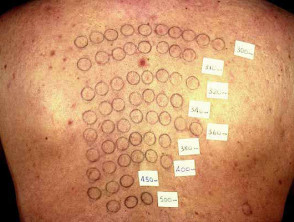
Phototesting
Sunburn
Sunburn is maximal about eight hours after exposure to ultraviolet radiation from sunlight or artificial sources (predominantly UVB). Features include:
- Pruritic and painful erythema, oedema, vesicles, and bullae in affected areas
- Sunburn is confined to exposed sites (but this may include skin covered by light clothing)
- Symptoms may be accompanied by headache, fever, lassitude
- The burn is followed within days by peeling and subsequently dyspigmentation (sunburn does not scar)
- Sunburn depends on skin phototype arising particularly rapidly in Type 1 skin
- Subsequent tan depends on phototype and does not occur in Type 1 skin
Sunburn arises with less exposure to sunlight when the patient is taking phototoxic drugs (sulphonamides, thiazides, tetracyclines, phenothiazines, nalidixic acid, amiodarone, naproxen and psoralens). Consider systemic lupus erythematosus in the differential diagnosis.
The histology is characterised by “sunburn” cells (apoptotic keratinocytes), lymphocytic exocytosis, vacuolisation of melanocytes and endothelial swelling of blood vessels.
Prevention of sunburn requires the use of covering clothing, sunscreens and perhaps oral antioxidants such as Polypodium leucotomas. Treatment may consist of rest, fluid replacement, cooling wet dressings, topical steroids and NSAIDs.
Sunburn and phototoxicity
Photocontact dermatitis
Photocontact dermatitis (eczema) refers to dermatitis arising from contact with a photoactive chemical when exposed to light.
- Photocontact dermatitis may be due to photoirritant and/or photoallergic mechanisms.
- The result is a typical dermatitis following exposure to UVA entirely or predominantly affecting sun-exposed sites.
- Common causes include creosote, coal tar, sunscreens, topical NSAIDs and antimicrobial agents (e.g. in antiseptic soaps).
- It should be managed with sun protection, avoidance of the responsible agent and topical steroids.
Photocontact reactions
Phytophotodermatitis
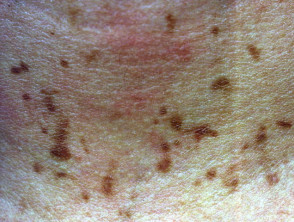
Plant photocontact dermatitis, or phytophotodermatitis, is due to photoactive psoralens (as used for PUVA treatment), found in limes, perfumes containing oil of bergamot and celery.
- Phytophotodermatitis typically results in linear blisters and erythematous plaques, but a buckshot appearance may follow use of a string trimmer to clear umbelliferae weeds such as wild carrot.
- The acute eruption may be followed by prolonged pigmentation.
Phytodermatitis
Drug-induced photosensitivity
Drug-induced systemic photoallergy may have various patterns, most often an eczematous dermatitis or a lichenoid eruption (i.e. having histological features similar to lichen planus). Photosensitivity affecting the nails results in lifting of the nail plate off the nail bed (photo-onycholysis) and may take many months to recover.
- Drug-induced photosensitivity eruptions are usually provoked by UVA so may arise through window glass
- The eruptions may be uniform or patchy
- They should be managed by drug withdrawal, photoprotection and topical steroids
- Rarely, drug-induced photosensitivity can result in persistent light eruption (i.e. the rash does not clear on drug withdrawal)
Drug-induced photosensitivity
Photo-aggravated dermatoses
Photo-aggravated dermatoses include:
- Connective tissue diseases especially cutaneous lupus erythematosus, dermatomyositis
- Photo-aggravated atopic dermatitis or psoriasis
- Photosensitivity is generally preceded by quite typical atopic dermatitis or psoriasis
- Photosensitivity is often broad spectrum (UVB and UVA)
- The relationship to sun exposure is often unrecognised by patient and doctor
- Genodermatoses: Darier disease, disseminated superficial actinic porokeratosis (DSAP), porphyrias and others
- Miscellaneous dermatoses including herpes simplex and pellagra
Management involves treating the underlying disease and photoprotection.
Photo-aggravated dermatoses
Polymorphous light eruption
Polymorphous light eruption (PMLE) is a common idiopathic photosensitivity eruption affecting young adult women. Features include:
- The rash usually spares habitually exposed areas (face, hands)
- A variant affecting the tops of the ears of young boys is called Juvenile spring eruption
- PMLE presents after several hours exposure to spring or summer sun and persists for several days
- It may occur once or recur throughout summer each year
- Irritable clustered papules or papulovesicles are the most common variant but eczematous plaques or erythema multiforme-like lesions occur in some patients
PMLE should be managed by sun protection, with a gradual increase in exposure. Some patients find antioxidants such as beta carotene or Polypodium leucotomas of benefit. Severe cases may be referred to a dermatologist. Treatment options include:
- Hydroxychloroquine
- Phototherapy (usually UVB)
- Photochemotherapy (PUVA)
- Systemic steroids to cover holidays
Polymorphic light eruption
Rare idiopathic photodermatoses
Actinic prurigo
Actinic prurigo affects atopic children causing cheilitis and itchy papules predominantly on exposed sites.
Actinic prurigo
Actinic prurigo affects atopic children causing cheilitis and itchy papules predominantly on exposed sites.
Hydroa vacciniforme
Hydroa vacciniforme causes clear vesicles on the cheeks of children.
Chronic photosensitivity dermatitis
Chronic photosensitivity dermatitis (CPD) mainly affects elderly men and may result in extreme photosensitivity (30 seconds exposure outdoors in winter may be enough). Severe CPD results in lymphoma-like thickened plaques and is known as actinic reticuloid.
Solar urticaria
Solar urticaria is a physical urticaria provoked by a few minutes exposure to responsible wavelengths.
Hydroa vacciniforme
Hydroa vacciniforme causes clear vesicles on the cheeks of children.
Chronic photosensitivity dermatitis
Chronic photosensitivity dermatitis (CPD) mainly affects elderly men and may result in extreme photosensitivity (30 seconds exposure outdoors in winter may be enough). Severe CPD results in lymphoma-like thickened plaques and is known as actinic reticuloid.
Solar urticaria
Solar urticaria is a physical urticaria provoked by a few minutes exposure to responsible wavelengths.
Rare idiopathic photodermatoses
Photoprotection
Patient education is important to explain that photosensitivity may occur throughout the year, behind glass and provoked by natural and artificial sources of light. The best protection is to stay indoors, especially during the middle part of the day. Additional measures outdoors may include:
- Fully covering clothing and a broad-brimmed hat.
- Sunscreens, but they may appear ineffective. Select a broad-spectrum ‘ultra’ formula with very high protection factor (some are measured as SPF100+), and water resistant properties. Apply to all uncovered skin first thing and reapplied two-hourly if outdoors at all.
Severely photosensitive patients may require immunosuppressive medication, window screening, gloves and masks.
Photoprotection
Activity
Compile a list of high sun protection factor, water resistant sunscreens available in your local pharmacy that are suitable for patients with photosensitivity.
Related information
References:
On DermNet NZ:
Information for patients
Other websites:
- Medscape Reference: Photo-related Diseases
- Medscape: Drug-Induced Photosensitivity Journal article 1998
- Merck Professional: Photosensitivity
Books about skin diseases:
See the DermNet NZ bookstore
Sign up to the newsletter
© 2024 DermNet.
DermNet does not provide an online consultation service. If you have any concerns with your skin or its treatment, see a dermatologist for advice.