Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Ectodermal dysplasia is a large group of inherited disorders characterised by a primary defect in hair, teeth, nails or sweat gland function, in addition to another abnormality in any tissue of ectodermal origin. These are ears, eyes, lips, mucous membranes of the mouth or nose, and the central nervous system.
The ectoderm is the outermost layer of cells in embryonic development and contributes to the formation of many parts of the body including all those described above. Ectodermal dysplasia occurs when the ectoderm of certain areas fails to develop normally. All ectodermal dysplasias are present from birth and are non-progressive.
Currently, there are about 150 different types of ectodermal dysplasias. In an attempt to classify these, different subgroups are created according to the presence or absence of the four primary ectodermal dysplasia (ED) defects:
Based on the above, the 150 different types of ectodermal dysplasias are categorised into one of the following subgroups made up from the primary ED defects:
The most common ectodermal dysplasias are hypohidrotic (anhidrotic) ED which falls under subgroup 1-2-3-4 and hydrotic ED which comes under subgroup 1-2-3.
The three most recognised ectodermal dysplasia syndromes fall into the subgroup 1-2-3-4, as they show features from all four of the primary ED defects. They are:
Prenatal testing is available for ectodermal dysplasia syndromes in some centres.
The different types of ectodermal dysplasia are caused by the mutation or deletion of certain genes located on different chromosomes. Because ectodermal dysplasias are caused by a genetic defect, they may be inherited or passed on down the family line. In some cases, they can occur in people without a family history of the condition, in which case a de novo mutation has occurred.
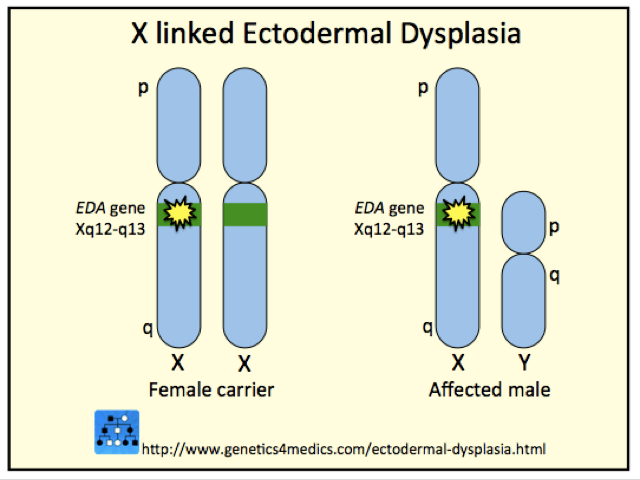
Ectodermal dysplasia genetics*
*Image courtesy Genetics 4 Medics
The signs and symptoms of ectodermal dysplasia differ markedly between the different types and depend on the structures that are affected. Signs and symptoms are not usually apparent in newborns and may not be picked up till infancy or childhood.

Anhidrotic ectodermal dysplasia
Ectodermal dysplasia typically affects the four organs primarily involved in the following ways:
| Affected organ | Features |
|---|---|
| Hair | - Scalp and body hair may be thin, sparse, and light in colour - Hair may be coarse, excessively brittle, curly or even twisted |
| Nails | - Fingernails and toenails may be thick, abnormally shaped, discoloured, ridged, slow-growing, or brittle - Sometimes nails may be absent - Cuticles may be prone to infection |
| Teeth | - Abnormal tooth development resulting in missing teeth or growth of teeth that are peg-shaped or pointed - Tooth enamel is also defective - Dental treatment is necessary and children as young as two years may need dentures |
| Sweat glands | - Eccrine sweat glands may be absent or sparse so that sweat glands function abnormally or not at all - Without normal sweat production, the body cannot regulate temperature properly - Children may experience recurrent high fever that may lead to seizures and neurological problems - Overheating is a common problem, particularly in warmer climates |
Other signs and symptoms include:
There is no specific treatment for ectodermal dysplasia. Management of the condition is by treating the various symptoms. Patients often need to be treated by a team of doctors and dentists, rather than a sole practitioner.
Most people with ectodermal dysplasia can lead a full and productive life once they understand how to manage their condition. Special attention must be paid to children if sweating and mucus production abnormalities are present. Recurrent high fevers may lead to seizures and neurological problems.