Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Author: Honorary Associate Profesor Amanda Oakley, Dermatologist, Hamilton, New Zealand, 1998. Further updates: December 2015 and May 2023.
Introduction
Demographics
How hair grows
Causes
Clinical features
Complications
Diagnosis
Treatment
Prevention
Outlook
The medical term for hair loss is alopecia. There may be associated scalp disease or scarring.
Unfortunately, hair loss may not be easy to remedy.
As all our hair follicles are formed during fetal growth, it is inevitable that we will notice hair loss of some kind in later life.
Hair loss occurs in:
Hair loss can be an isolated problem or associated with another disease or condition. It can be temporary or permanent, depending on the cause.
Hair grows on most parts of the skin surface, except palms, soles, lips and eyelids. Hair thickness and length varies according to the site.
A hair shaft grows within a follicle at a rate of about 1 cm per month. It is due to cell division within the hair bulb at the base of the follicle. The cells produce the three layers of the hair shaft (medulla, cortex, cuticle), which are mainly made of the protein keratin (which is also the main structure of skin and nails).
Hair growth follows a cycle. However, these phases are not synchronised, and any hair may be at a particular phase at random.
The three main phases of the hair cycle are:
Hair length depends on the duration of anagen. Short hairs (eyelashes, eyebrows, hair on arms and legs) have a short anagen phase of around one month. Anagen lasts up to 6 years or longer in scalp hair.
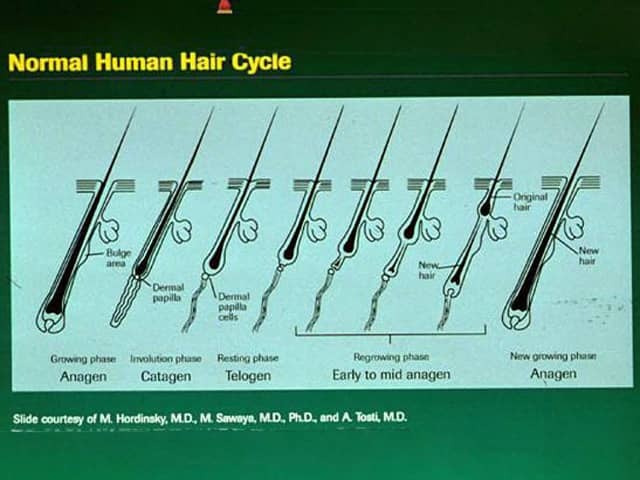
Image © 1998 Merck Sharpe and Dohme (with permission)
Hair loss can be due to:
The features of hair loss depend on the cause. Actual symptoms such as itch and soreness are generally absent unless caused by accompanying inflammatory skin disease. However, a burning, prickly discomfort known as trichodynia may accompany hair shedding.
Anagen hair is tapered or broken-off. Anagen is variable in duration. Children with otherwise normal hair but that cannot grow their hair long may have short anagen syndrome.
Anagen shedding is known as anagen effluvium and has a sudden onset.
Anagen effluvium is caused by:
Short broken hairs and empty follicles may be observed. If caused by a drug or toxin, hair growth can return to normal within 3–6 months of its withdrawal.

Hair shedding during chemotherapy

Hair lost through chemotherapy

Alopecia areata
Telogen hair has a bulb at the end (club hair). Excessive shedding is known as telogen effluvium. It occurs 2–6 months after an event that stops active hair growth.
Telogen effluvium is caused by:
Sometimes there appears to be no recognisable cause for telogen effluvium, and shedding can continue for years (chronic telogen effluvium). Scalp hair continues to grow but has a shorter natural length than normal.

Telogen effluvium

Telogen effluvium
Pattern hair loss is due to genetic programming or hormonal influences. It is also called androgenetic alopecia because it is influenced by androgens.
Pattern alopecia is apparent in about 50% of individuals by the age of 50 years.

Male pattern balding

Female pattern balding

Severe female pattern balding
Hair shaft defects can be inherited and congenital, or acquired due to disease or injury (eg, excessive brushing, hair pulling [trichotillomania], hairdryer heat, relaxing chemicals, bleach). See African hair practices.
Hair shaft abnormalities are diagnosed by dermatoscopy or microscopic examination of the hair, and sometimes by scanning electron microscopy. They include:
Conditions resulting in reversible patchy hair thinning, poor hair quality and bald patches include:

Tinea capitis

Psoriasis © R Suhonen

Seborrhoeic dermatitis
Systemic diseases resulting in reversible patchy hair thinning, poor hair quality and bald patches include:
Inflammation in the dermis or subcutaneous tissue may injure the hair follicle resulting in localised bald patches in which there are no visible follicles; this is called scarring alopecia or cicatricial alopecia.
Traumatic causes of scarring alopecia may be due to:

Trichotillomania

Trichotillomania

Traction alopecia
Infections causing scarring alopecia include:
Inflammatory skin diseases causing scarring alopecia include:
Pseudopelade of Brocq is a condition in which there are localised areas of the scalp in which hair follicles have disappeared without visible inflammation.

Discoid lupus erythematosus

Folliculitis decalvans

Lichen planopilaris
Whatever the type of hair loss, it may be extremely distressing and embarrassing, reducing the quality of life and causing psychosocial problems. Loss of normal scalp hair increases the risk of:
A careful history and full skin examination can generally result in the correct diagnosis. Additional tests may include:
Treatment depends on the diagnosis.
A systematic review of 30 studies suggests a discussion on nutritional supplementation should be considered between patient and physician.
For specific treatments, see individual pages for the different types of alopecia.
Most types of hair loss cannot be actively prevented. However, it is prudent to avoid injury to the hair shaft.
The outlook for hair loss depends on the diagnosis. Scarring alopecia is permanent.