Fibroblastic connective tissue naevus typically presents in the first decade of life, often as a poorly defined plaque-like cutaneous thickening arising most commonly on the trunk and head/neck of girls.
Histology of fibroblastic connective tissue naevus
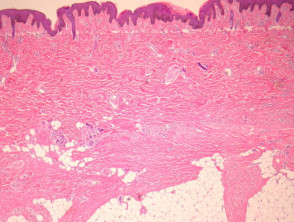
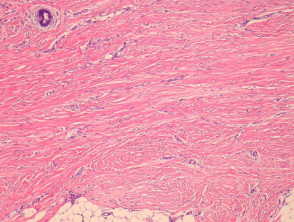
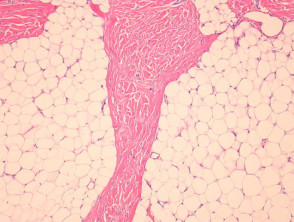
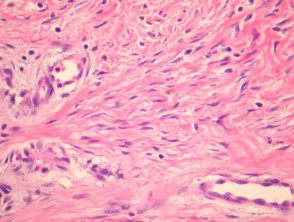
Fibroblastic connective tissue naevus is situated primarily in the reticular dermis, and often shows extension into the superficial subcutis (figures 1, 2). There may be a mild papillomatous epidermis. The lesional cells are bland spindle-shaped fibroblastic/myofibroblastic cells with indistinct pale eosinophilic cytoplasm and tapering nuclei, with no significant cytologic atypia or pleomorphism (figures 3, 4). These cells form short fascicles with no particular orientation to the overlying epidermis and are associated with a loose stroma composed of mainly delicate or wispy collagen bundles (figures 3, 4).
Fibroblastic connective tissue naevus pathology
Special studies for fibroblastic connective tissue naevus
The lesion cells show variable expression of CD34. Smooth muscle actin shows variable positivity. FISH studies fail to reveal the PDGF/Col translocation seen in dermatofibrosarcoma.
Differential diagnosis of fibroblastic connective tissue naevus
Dermatofibrosarcoma protuberans – These are usually more cellular and show a storiform growth pattern. FISH studies typically reveal a PDGF/Col translocation.