Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Author: Dr Susan Simpkin, Dermatology Registrar, Auckland, New Zealand, 2011.
Introduction
Introduction - alcohol abuse
Associated health problems
Chronic alcohol abuse
Vascular effects
Skin changes due to liver disease
Skin cancer
Nutritional deficiency
Oral changes
Skin conditions
Alcohol sensitivity
Alcohol and medications
Excessive alcohol (ethanol) intake or alcohol abuse can result in many health problems and is implicated as a cause or aggravating factor for several skin conditions.
Alcohol abuse has been defined as recurrent alcohol use where it impacts on work, school or home, or to the point it is physically dangerous, gets you into trouble with the law, or continues despite the problems it has created.
Effects of alcohol intoxication include:
Effects of chronic alcohol abuse include:
This infographic shows effects of alcohol on the body.
One of the earliest signs of alcohol abuse is a persistently red face due to enlarged blood vessels (telangiectasia). This appears because regulation of vascular control in the brain fails with sustained alcohol intake.
Transient flushing is also a common side effect of alcohol, particularly in heavy drinkers. It is due to acetaldehyde, the main breakdown product of alcohol. Acetaldehyde is thought to cause flushing by stimulating release of histamine.
Up to 40% of northeastern Asians experience flushing and elevated heart rate after drinking even minimal amounts of alcohol, due to accumulation of acetaldehyde. This is because of a mutation in acetaldehyde dehydrogenase (ALDH2), the enzyme that converts acetaldehyde to acetate.

Facial redness

Telangiectasia

Flushing
Spider telangiectasis is given that name because of its appearance. Blood vessels (the spider legs) radiate out in all directions from a central blood vessel (its body). Like other blood vessels, spider angiomas blanch when pressure is applied. They may pulsate. They are most frequently found on the face, v of the neck, chest, arms, hands and abdomen.
Large numbers of spider telangiectases are associated with liver cirrhosis (scarring of the liver) due to elevated oestrogen levels. A study of 82 patients with liver cirrhosis showed significantly higher numbers of spider telangiectases in alcoholic cirrhotic patients than non-alcoholic cirrhotic patients, indicating there may be an additional effect such as vasodilation to account for this difference.
Small numbers of spider telangiectases are seen in healthy children and adults. They are more common in women, especially during pregnancy, as they are influenced by the female hormone, oestrogen.
Chronic alcoholic liver disease may lead to reddening of palmar skin. This is also thought to be due to oestrogen, as it sometimes observed during normal pregnancy.
High pressure within the venous system in the liver leads to high pressure in the venous system elsewhere in the body including the veins around the umbilicus (belly button). When these veins are dilated the appearance has been likened to ‘caput medusa’ (head of Medusa), referring to Greek mythology where a once beautiful woman was cursed and her hair turned into snakes.
The skin and sclera of the eyes often turn yellow in patients with alcoholic liver disease. The colour, known as jaundice, is due to bilirubin, a product broken down from haem derived from red blood cells. The metabolism of bilirubin is impaired in acute and chronic liver disease. Jaundice lessens as liver function improves.

Spider telangiectases

Palmar erythema

Skin darkening (hyperpigmentation) around the eyes, mouth and on the legs may be associated with chronic liver disease. The reason this occurs is unclear.
Generalised skin itching (pruritus) may occur due to the build up of poorly metabolised substances that stimulate nerve endings in the skin. These substances may include bile salts, histamine, corticosteroids and opioids.
Nail changes associated, but not specific to alcohol-related liver disease include:

Clubbing

Koilonychia

Muehrcke nail
Porphyria cutanea tarda (PCT) results in photosensitivity, skin fragility, blistering, erosions, crusts, milia, scleroderma and increased hair growth (hypertrichosis) on sun-exposed sites such as face and hands.
Alcohol is the most common cause of acquired or type 1 PCT in susceptible individuals and is associated with chronic liver disease. Porphyrins build up because of deficiency in uroporphyrinogen decarboxylase (UROD), an enzyme important in the sythesis of the blood protein haem.
Other factors that may trigger type 1 PCT include oestrogen, iron and viral infections (especially hepatitis C). Familial or type 2 PCT is due to genetic deficiency in UROD.

Porphyria cutanea tarda

Porphyria cutanea tarda

Porphyria cutanea tarda
Along with increasing the risk of liver, pancreatic, and breast cancer, alcohol increases the risk of skin cancer including squamous cell carcinoma, basal cell carcinoma, and melanoma. Alcohol is also associated with an increased risk of oral cancer.
The reasons why excessive alcohol consumption may cause cancer include:

Squamous cell carcinoma

Basal cell carcinoma
Oral squamous cell carcinoma
Nutritional deficiency can develop when alcohol replaces normal food in the diet and the digestive tract and liver do not digest and process food the way they should resulting in malabsorption. With little calorie or protein intake the skin becomes dry and loses elasticity.
Vitamins are essential to maintain healthy looking skin:

Dry skin

Follicular keratosis

Angular cheilitis
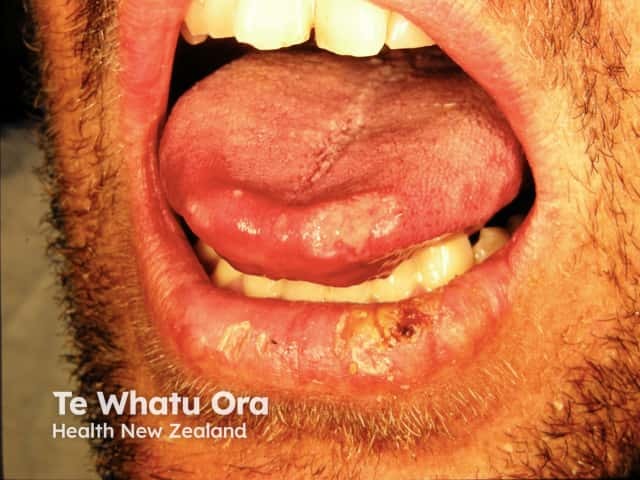
Changes found in the mouth often relate to nutritional deficiency or poor oral hygiene. These include:
In addition, swelling of the parotid gland may be a result of chronic alcohol use.
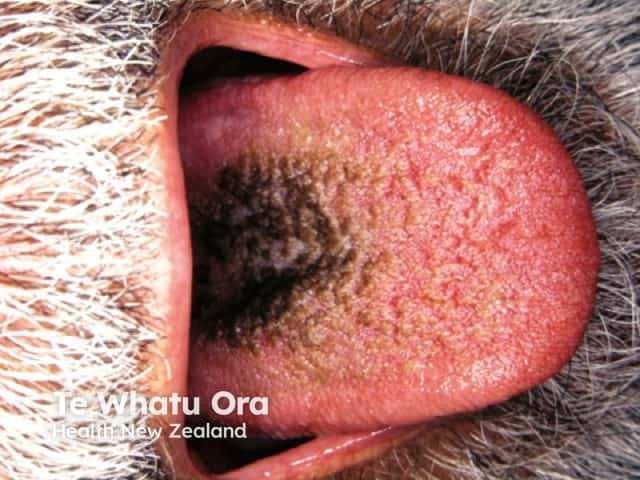
Black hairy tongue

Black hairy tongue

Parotid swelling
All of these skin conditions may occur without any history of alcohol abuse.
Alcohol induces vasodilation and facial flushing in people who have rosacea. However, alcohol is not the cause of the skin disease in most people.
Although the classic ‘drinker's nose’ (rhinophyma) was thought to be related to excess alcohol consumption, it has never been proven. In a case-control study of 175 people with rosacea and 145 people with normal skin, there was no significant difference in alcohol consumption between the two groups.

Telangiectatic rosacea

Papulopustular rosacea

Rhinophyma
High intake of alcohol is a risk factor for new onset of psoriasis. The distribution of psoriasis has been observed to be particularly prominent on the fingers and hands of heavy drinkers. People who have psoriasis and drink more than 80g of alcohol per week have been found to have more severe treatment-resistant psoriasis, including erythrodermic psoriasis. The reasons for the association may be relative immune suppression induced by alcohol and/or that it induces proinflammatory cytokines.
Heavy drinking reduces options for treatment of psoriasis, as some medicines are contraindicated if the drinking has led to liver disease (methotrexate) or to high levels of triglyceride (acitretin). Patients with psoriasis and high alcohol intake are also more likely to suffer from depression.

Scalp psoriasis

Chronic plaque psoriasis

Flexural psoriasis
Seborrhoeic dermatitis has been observed to be more frequent in heavy drinkers.

Seborrhoeic dermatitis

Rosacea

s
Nummular or discoid dermatitis occurs more frequently in alcohol abusers, particularly in those with abnormal liver function tests.

Nummular dermatitis

Nummular dermatitis

Nummular dermatitis
Skin infections occur more frequently in patients who drink alcohol excessively due to impairment of the immune system, nutritional deficiency and increased trauma. These include:
Bacterial skin infections that may lead to septicaemia (spread to the blood):
Fungal skin infectionsare common but rarely cause sepsis. They include:
Tuberculosis is also seen more frequently in alcoholics. Skin involvement is called cutaneous tuberculosis.

Wound infection

Cellulitis

Widespread tinea corporis
Urticaria (hives) may occur within minutes to hours of drinking alcohol and is sometimes due to allergic reaction. Flushing and overheating after drinking alcohol may also indicate cholinergic urticaria. This is a physical type of urticaria is brought on my heat, exercise, or stress.



Targetoid lesion in urticaria
Alcohol can give rise to allergic or allergy-like symptoms. Along with urticaria (see above), patients may develop low blood pressure, diarrhoea, shortness of breath, and low heart rate (anaphylaxis). Even tiny amounts of alcohol may induce urticaria in people who have had a severe reaction previously, although allergy testing is often negative.
Some apparent allergic reactions to alcohol are due to inherited defects in alcohol metabolising enzymes or allergy to other contents or additives in the drink such as colouring agents, preservatives, or flavouring.
Some medicines used to treat dermatological disorders should not be taken with alcohol. Examples include: