What is Peutz-Jeghers syndrome?
Peutz-Jeghers syndrome (PJS) is a rare inherited disease that is characterised by gastrointestinal polyps in association with pigmentation affecting skin and mucous membranes.
PJS polyps are hamartomas i.e. benign tumours made up of a mixture of mature cells normally found in that tissue. They can show benign (non-cancerous) or malignant (cancerous) changes. The risk of developing some form of internal cancer is 15 times greater for patients with PJS compared with the general population.
What is the cause?
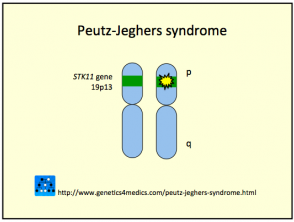
Peutz-Jeghers syndrome is due to germ line mutations in the Serine Threonine Kinase tumor-suppressor gene found on chromosome 19p13.3 (also called STK11/LKB1). The gene abnormality may be inherited or arise sporadically (35%). The key factor may be reduced apoptosis, or programmed cell death, in the affected cells.
PJS has autosomal dominant inheritance. This means that offspring of affected individuals have a 50% chance of inheriting the disease.
Genetics of Peutz-Jeghers syndrome*
*Image courtesy Genetics 4 Medics
What are the clinical features of Peutz-Jeghers syndrome?
Clinical features of PJS can be divided into two types, cutaneous and gastrointestinal.
Cutaneous features
The most noticeable cutaneous feature of PJS is the appearance of melanocytic macules (pigmented spots) in 95% of patients. Tan, dark brown, or bluish black flat patches 1 to 5 mm in size are seen around the mouth, lips, gums, inner lining of the mouth, eyes, hands and feet, fingers and toes, anus and genital areas. Pigmentation usually appears before 5 years of age and may fade after puberty.
Gastrointestinal features
Gastrointestinal polyps occur later on in life and are rare in childhood. The polyps may cause bleeding and abdominal pain. They have a high chance of becoming malignant.
Small intestine intussusception (when one portion of an intestine protrudes into another) and intestinal obstruction are also fairly common complications of Peutz-Jeghers syndrome.
How is Peutz-Jeghers syndrome diagnosed?
The diagnosis is suspected when there are typical clinical features. Laugier-Hunziker syndrome presents with similar pigmented macules around and inside the mouth, but often also presents with melanonychia (longitudinal pigmented bands on one or more nails). Laugier-Hunziker syndrome is not associated with STK11 gene mutations.
Diagnostic work-up should include:
- Clinical assessment of pigmentary lesions
- Complete blood cell (CBC) count as polyps may bleed leading to anaemia
- Exploratory endoscopy to determine the presence and location of polyps
- Pathological examination of polyps to confirm diagnosis
- STK11 gene testing, if available
What is the treatment for Peutz-Jeghers syndrome?
Approximately 50% of patients with PJS develop and die from cancer by 57 years of age. The overall risk of Peutz-Jeghers syndrome patients developing a cancer over adult life is 93%. Cancers are not only located on the gastrointestinal tract but can occur on many other sites including the breast, ovary, testicle, pancreas, uterus, oesophagus, and lung.
There is no specific treatment for PJS but the main goal is to manage and prevent associated problems of intestinal obstruction and intussusception, and cancer development.
Management of PJS patients should include:
- Annual CBC
- Annual physical examination of breasts, abdomen, pelvis and testes
- Repeated removal of bleeding or large polyps (>5 mm) by endoscopic polypectomy
- Laparotomy and resection as required for repeated or persistent intestinal intussusception, obstruction, or persistent bleeding
- Surgical removal of cancers as they are diagnosed
DNA screening may be offered to family members to see if they have inherited the gene mutation. If so, they should also undergo regular screening for disease.
The freckling may be less obvious with careful sun protection. In some cases, the pigmentation may be lessened by cosmetic treatment. Cosmetic camouflage may also be useful.