What is angular cheilitis?
Angular cheilitis is a common, non-contagious, inflammatory condition affecting the corners of the mouth or oral commissures.
Depending on the underlying cause, it may last a few days or persist indefinitely. It is also called angular stomatitis, cheilosis, rhagades, or perleche (perlèche).
Bilateral angular cheilitis with grey maceration at the angles of the mouth An edentulous woman with redness and oozing in the lateral oral creases due to angular cheilitis
Crusting, oozing, and redness on the angle of the mouth
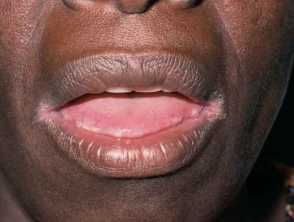
Angular cheilitis in skin of colour
Angular cheilitis in a denture wearer
Redness and erosion of the lateral oral skin folds in an edentulous woman
Angular cheilitis





Who gets angular cheilitis?
Angular cheilitis is common and can affect any child or adult. Those with poor health are especially susceptible.
Risk factors include:
- Dry chapped lips of any cause
- Oral thrush — this is more likely to occur in infancy, old age, diabetics, concurrent corticosteroid use or antibiotic use, and immunocompromised patients
- Dentures (especially if ill-fitted and there is associated gum recession)
- Poor nutrition — coeliac disease, iron deficiency, riboflavin deficiency, general protein deficiency, zinc deficiency, vitamin B12 and/or folate deficiency
- Systemic illness, particularly inflammatory bowel disease (ulcerative colitis and Crohn disease) and Sjogren syndrome
- Sensitive skin, especially atopic dermatitis
- Genetic predisposition — eg, in Down syndrome
- Oral retinoid medication — can cause dry lips, eg, isotretinoin, acitretin
- Rapid weight loss — leads to reduced skin turgor/elasticity and increased skin folds
- Smoking — reduces skin turgor/elasticity
- Retrognathia (abnormal posterior/set-back position of the jaw)
- An overhang of the upper lip resulting in deep furrows (marionette lines).
It is made worse by licking the lips.
What causes angular cheilitis?
Angular cheilitis occurs at the angles of the mouth where two different types of skin lining meet and act as a hinge. The lining of the oral cavity (oral mucosa) meets with squamous epithelium (facial skin). As they are used often for eating, drinking, and talking, they are vulnerable to stress/trauma.
Angular cheilitis most commonly occurs due to prolonged exposure of the corners of the mouth to saliva and its digestive enzymes, resulting in eczematous cheilitis (a form of irritant contact dermatitis)
What are the clinical features of angular cheilitis?
Angular cheilitis may result in the following symptoms and signs at the corners of the mouth:
- Painful cracks/fissures worse on mouth opening
- Blisters, erosions, oozing, crusting
- Redness (or pallor/darkening of the skin in some cases)
- Bleeding.
It is usually bilateral and symmetrical, however, it can occur on one side. It may progress to more widespread impetigo or candidiasis (oral thrush) on the adjacent skin and elsewhere.
How do clinical features vary in differing types of skin?
Angular cheilitis in dark skin may be more subtle in the initial stages, or the skin may appear pale rather than reddened. The pale areas of skin may also be surrounded by a darkened rim.
What are the complications of angular cheilitis?
- Rarely, if chronic or left untreated, angular cheilitis can cause permanent scarring and discolouration of the skin.
- If the cause is a bacterial infection, there is a risk of the infection spreading to nearby skin.
- Risk of subsequent infection such as fungal infection, oral thrush.
How is angular cheilitis diagnosed?
Angular cheilitis is diagnosed clinically based on history and examination.
The culture of swabs taken from the corners of the mouth may reveal:
Skin biopsy is not usually necessary.
What is the differential diagnosis for angular cheilitis?
- Impetigo
- Atopic dermatitis
- Seborrheic dermatitis
- Allergic contact dermatitis
- Irritant contact dermatitis
- Secondary syphilis/syphilitic papule (more likely unilateral)
- Early or isolated diffuse cheilitis
- Erosive oral lichen planus
What is the treatment for angular cheilitis?
In many cases, no treatment is needed and angular cheilitis resolves by itself.
General measures
- Improved general hydration
- Use of lip balm or a thick emollient ointment applied frequently (often sufficient treatment alone for saliva-induced angular cheilitis)
- Topical antiseptics
Specific measures
Depending on the specific cause, oral and topical treatment options include:
- Topical antifungal cream
- Oral antifungal medication
- Topical or oral antistaphylococcal antibiotic
- Topical steroid ointment if the skin is significantly inflamed.
How do you prevent angular cheilitis?
- Education around reduced licking of the lips
- Nutritional supplements
- Quitting smoking of cigarettes
- Replacement of ill-fitted dentures to normalise face contour and reduce the size of mouth furrows
- Use of topical emollients/lip balm to keep lips from being too dry
- Rinsing the mouth after use of inhaled corticosteroids
- Maintaining good oral and denture hygiene
- Filler injections or implants to build up the oral commissures
- Improved blood glucose control in those with diabetes mellitus
- Botulinum toxin to smooth out mouth furrows
What is the outcome for angular cheilitis?
In many cases angular cheilitis self-resolves, if not it is usually curable and rarely results in permanent scarring or pigmentation. Improvement is usually seen within the first few days of treatment and typically resolves by two weeks.
Repeat occurrences of angular cheilitis are common, especially in those with non-modifiable risk factors.