What is cutaneous lupus erythematosus?
Cutaneous lupus erythematosus (LE) is a diverse group of autoimmune connective tissue disorders localised to the skin that can be associated with systemic lupus erythematosus (SLE) to varying degrees.
Cutaneous lupus erythematosus (CLE) is classified as:
- Acute (ACLE)
- Subacute (SCLE)
- Intermittent (lupus tumidus)
- Chronic (CCLE) eg, discoid lupus (DLE), lupus profundus, chilblain lupus erythematosus.
Cutaneous lupus erythematosus
Skin lesions of cutaneous lupus erythematosus can be subdivided into:
- Lupus-specific changes
- Clinical signs diagnostic of, or unique to, LE
- Histology is diagnostic for LE; vacuolar interface dermatitis
- Lupus-nonspecific changes
- Clinical signs found not only in LE, but also in other connective tissue diseases
- Histology is not diagnostic for LE; reactive patterns seen.
Who gets cutaneous lupus erythematosus?
Cutaneous lupus erythematosus has an annual incidence of 4 cases per 100,000 people, and a prevalence of 73 cases per 100,000.
As with SLE, there is a marked female predominance with CLE particularly affecting women 20 to 50 years of age. However, all age groups and both sexes can be affected. Skin of colour is an important predisposing factor.
Up to 75% of patients with SLE develop cutaneous signs, and these may be the first indication of SLE in 25%.
What causes cutaneous lupus erythematosus?
The pathogenesis of cutaneous lupus erythematosus is multifactorial:
- Genetic susceptibility
- High incidence among family members
- Environmental factors
- Cigarette smoking
- Sun exposure
- Medications
- Innate and adaptive immune responses
- autoantibodies.
What are the clinical features of cutaneous lupus erythematosus?
This is a brief overview of the clinical features of cutaneous lupus erythematosus. See the specific lupus pages for more detail – links are provided at the end under the ‘On DermNet’ heading.
Acute cutaneous lupus erythematosus
Acute cutaneous lupus erythematosus typically presents as transient erythematous patches associated with a flare of systemic lupus erythematosus.
Lupus-specific skin changes:
- Localised acute CLE: malar ‘butterfly' rash – redness and swelling over both cheeks, sparing the nasolabial folds, lasting hours to days
- Generalised acute CLE: diffuse or papular erythema of the face, upper limbs (sparing the knuckles), and trunk resembling a morbilliform drug eruption or viral exanthem
- Toxic epidermal necrolysis-like acute CLE: is associated with lupus nephritis or cerebritis, and must be distinguished from drug-induced toxic epidermal necrolysis in a patient with SLE.
Acute cutaneous lupus erythematosus
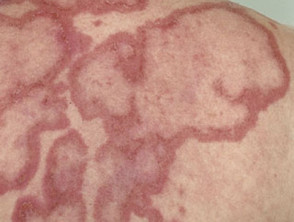
Subacute cutaneous lupus erythematosus
Subacute cutaneous lupus erythematosus is less commonly associated with SLE with approximately 50% having a mild form of SLE. It is thought 20–40% have drug-induced SCLE. It comprises 10–15% of cutaneous LE presentations. The skin changes are more persistent than those of ACLE.
Skin lesions of SCLE:
- Occur on the trunk and upper limbs, triggered or aggravated by sun exposure
- Present as a psoriasiform papulosquamous rash or annular, polycyclic plaques with central clearing
- Resolve to leave dyspigmentation and telangiectases, but no scarring.
Subacute cutaneous lupus erythematosus
Intermittent cutaneous lupus erythematosus
Intermittent CLE is better known as lupus tumidus, a dermal form of lupus erythematosus.
Skin lesions of lupus tumidus:
- Occur on sun-exposed areas of skin, such as the face, neck, and upper anterior chest
- Present as erythematous, round or annular, papules and plaques with a smooth surface
- Resolve in winter without scarring.
Lupus tumidus
Chronic cutaneous lupus erythematosus
Chronic cutaneous lupus erythematosus is the most common form of CLE, and about 25% of SLE patients have some form of CCLE.
Discoid lupus erythematosus
Discoid lupus erythematosus is the most common form of CCLE (80%) and is particularly prevalent and severe in patients with skin of colour. Only 1–2% of patients with localised DLE progress to SLE.
Skin lesions of DLE:
- Are most commonly located on the scalp, ears, cheeks, nose, and lips
- Present as destructive scaly plaques with follicular prominence (carpet tack sign) which can result in scarring alopecia
- Heal slowly leaving post-inflammatory dyspigmentation and scarring.
Discoid lupus erythematosus
Lupus profundus
Lupus profundus is a mostly lobular panniculitis without vasculitis.
Skin lesions of lupus profundus:
- Can develop at any site
- Present as persistent, firm, deep, tender nodules
- Resolve to leave dents in the skin due to atrophy of the fat.
Lupus profundus
Chilblain lupus erythematosus
Chilblain lupus erythematosus is an under-reported form of chronic CLE involving mainly the fingers and toes of smokers triggered by exposure to a moist cold environment. It may be familial with no association to SLE, or sporadic which can be associated with SLE.
Skin lesions of chilblain lupus:
- Are often pruritic and painful
- May ulcerate or develop hyperkeratotic fissuring
- May heal leaving depigmentation and atrophic spindling of the distal phalange.
Chilblain lupus erythematosus
How do clinical features vary in differing types of skin?
Some forms of cutaneous lupus erythematosus, such as bullous lupus erythematosus and discoid lupus erythematosus, are particularly associated with skin of colour.
Dyspigmentation and scarring are complications of CLE that significantly impact quality of life for patients with skin of colour.
Cutaneous lupus erythematosus in skin of colour
Non-specific cutaneous lupus erythematosus
- Non-scarring diffuse hair loss (unruly lupus hair)
- Raynaud phenomenon
- Livedo reticularis
- Nailfold telangiectases
- Photosensitivity
- Bullous systemic lupus erythematosus
- Mouth ulcers and cheilitis.
Non-specific skin signs of systemic lupus erythematosus
What are the complications of cutaneous lupus erythematosus?
- Progression to SLE and the complications of SLE
- Dyspigmentation [see Postinflammatory hyperpigmentation]
- DLE
- Scarring
- Permanent (cicatricial) hair loss
- Cutaneous squamous cell carcinoma
- Neonatal lupus erythematosus in baby of female patient with Ro and/or La autoantibodies
- Impact on quality of life [see Psychological effects of cutaneous lupus erythematosus]
Complications of cutaneous lupus erythematosus
How is cutaneous lupus erythematosus diagnosed?
- Skin biopsy — diagnostic histopathology and direct immunofluorescence is seen only in specific-LE lesions [see Discoid lupus erythematosus pathology]
- Blood tests — full blood count, renal function test, inflammatory markers
- Serology — including ANA, ENA – are often negative in chronic CLE
Cutaneous Lupus Erythematosus Disease Area and Severity Index (CLASI)
The Cutaneous Lupus Erythematosus Disease Area and Severity Index scores activity and damage in each of 12 anatomical locations.
The total activity score:
- Degree of redness (0-3) and scale (0-2)
- Mucous membrane involvement (0-1)
- Recent hair loss (0-1), nonscarring alopecia (0-3)
Total damage score:
- Degree of dyspigmentation (0-2) and scarring (0-2)
- Persistence of dyspigmentation more than 12 months doubles the dyspigmentation score
- Scalp scarring (0, 3, 4, 5, 6).
What is the treatment for cutaneous lupus erythematosus?
General measures
- Sun protection and avoidance: SPF 50+ broad spectrum sunscreen, UPF 50+ sun-protective clothing
- Smoking cessation
- Vitamin D supplement
Specific measures
Local therapy
Systemic therapy
- Antimalarials, usually hydroxychloroquine
- Immune modulators such as methotrexate, mycophenolate, dapsone, ciclosporin; there is evidence of successful treatment with anifrolumab
- Systemic corticosteroids
- Anifrolumab is a type 1 interferon receptor subunit blocker that has shown efficacy in systemic lupus as well as severe cutaneous lupus erythematosus
What is the outcome for cutaneous lupus erythematosus?
Cutaneous lupus erythematosus can be the presenting sign of SLE, as in acute CLE, or may evolve into SLE.
Female patients with CLE and Ro/La autoantibodies should be advised of the risk their baby may have neonatal lupus erythematosus including congenital heart block.
Chronic CLE tends to follow a chronic relapsing course for years, with flares in spring and summer, and resolution with scarring if untreated.