What is a lentigo?
A lentigo is a pigmented flat or slightly raised lesion with a clearly defined edge. Unlike an ephelis (freckle), it does not fade in the winter months. There are several kinds of lentigo.
The name lentigo originally referred to its appearance resembling a small lentil. The plural of lentigo is lentigines, although “lentigos” is also in common use.
Who gets lentigines?
Lentigines can affect males and females of all ages and races. Solar lentigines are especially prevalent in fair skinned adults. Lentigines associated with syndromes are present at birth or arise during childhood.
What causes lentigines?
Common forms of lentigo are due to exposure to ultraviolet radiation:
- Sun damage including sunburn
- Indoor tanning
- Phototherapy, especially photochemotherapy (PUVA).
Ionising radiation, eg radiation therapy, can also cause lentigines.
Several familial syndromes associated with widespread lentigines originate from mutations in Ras-MAP kinase, mTOR signalling and PTEN pathways.
What are the clinical features of lentigines?
Lentigines have been classified into several different types depending on what they look like, where they appear on the body, causative factors, and whether they are associated to other diseases or conditions.
Lentigines may be solitary or more often, multiple. Most lentigines are smaller than 5 mm in diameter.
Lentigo simplex
- A precursor to junctional naevus
- Arises during childhood and early adult life
- Found on trunk and limbs
- Small brown round or oval macule or thin plaque
- Jagged or smooth edge
- May have a dry surface
- May disappear in time
Lentigo simplex
Solar lentigo
- A precursor to seborrhoeic keratosis
- Found on chronically sun exposed sites such as hands, face, lower legs
- May also follow sunburn to shoulders
- Yellow, light or dark brown regular or irregular macule or thin plaque
- May have a dry surface
- Often has moth-eaten outline
- Can slowly enlarge to several centimetres in diameter
- May disappear, often through the process known as lichenoid keratosis
- When atypical in appearance, may be difficult to distinguish from melanoma in situ
Solar lentigo
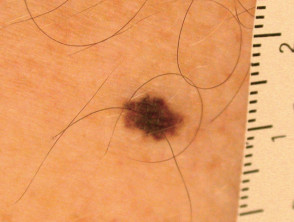
Ink spot lentigo
- Also known as reticulated lentigo
- Few in number compared to solar lentigines
- Follows sunburn in very fair skinned individuals
- Dark brown to black irregular ink spot-like macule
Ink spot lentigo
PUVA lentigo
- Similar to ink spot lentigo but follows photochemotherapy (PUVA)
- Location anywhere exposed to PUVA
PUVA lentigo
Tanning bed lentigo
- Similar to ink spot lentigo but follows indoor tanning
- Location anywhere exposed to tanning bed
Tanning bed lentigo
Radiation lentigo
- Occurs in site of irradiation (accidental or therapeutic)
- Associated with late-stage radiation dermatitis: epidermal atrophy, subcutaneous fibrosis, keratosis, telangiectasias
Melanotic macule
- Mucosal surfaces or adjacent glabrous skin eg lip, vulva, penis, anus
- Light to dark brown
- Also called mucosal melanosis
Melanotic macule
Generalised lentigines
- Found on any exposed or covered site from early childhood
- Small macules may merge to form larger patches
- Not associated with a syndrome
- Also called lentigines profusa, multiple lentigines
Generalised lentigines
Agminated lentigines
- Naevoid eruption of lentigos confined to a single segmental area
- Sharp demarcation in midline
- May have associated neurological and developmental abnormalities
Patterned lentigines
- Inherited tendency to lentigines on face, lips, buttocks, palms, soles
- Recognised mainly in people of African ethnicity
Centrofacial neurodysraphic lentiginosis
- Associated with intellectual disability
Lentiginosis syndromes
- Syndromes include LEOPARD/Noonan, Peutz-Jeghers, Laugier-Hunziker, Moynahan, Xeroderma pigmentosum, myxoma syndromes (LAMB, NAME, Carney), Ruvalcaba-Myhre-Smith, Bannayan-Zonnana syndrome, Cowden disease (multiple hamartoma syndrome )
- Inheritance is autosomal dominant; sporadic cases common
- Widespread lentigines present at birth or arise in early childhood
- Associated with neural, endocrine, and mesenchymal tumours
Multiple lentigines
See more images of lentigines ...
How is the diagnosis made?
Lentigines are usually diagnosed clinically by their typical appearance. Concern regarding possibility of melanoma may lead to:
- Dermatoscopy
- Diagnostic excision biopsy
Histopathology of a lentigo shows:
- Thickened epidermis
- An increased number of melanocytes along the basal layer of epidermis
- Unlike junctional melanocytic naevus, there are no nests of melanocytes
- Increased melanin pigment within the keratinocytes
- Additional features depending on type of lentigo
In contrast, an ephelis (freckle) shows sun-induced increased melanin within the keratinocytes, without an increase in number of cells.
What is the treatment for lentigines?
Most lentigines are left alone. Attempts to lighten them may not be successful. The following approaches are used:
- SPF 50+ broad-spectrum sunscreen
- Hydroquinone bleaching cream
- Alpha hydroxy acids
- Vitamin C
- Retinoids
- Azelaic acid
- Cysteamine cream
- Chemical peels.
Individual lesions can be permanently removed using:
- Cryotherapy
- Intense pulsed light
- Pigment lasers.
How can lentigines be prevented?
Lentigines associated with exposure ultraviolet radiation can be prevented by very careful sun protection. Clothing is more successful at preventing new lentigines than are sunscreens.
What is the outlook for lentigines?
Lentigines usually persist. They may increase in number with age and sun exposure. Some in sun-protected sites may fade and disappear.