What is photographic skin surveillance?
Photographic skin surveillance usually refers to a screening programme for those at high risk of malignant melanoma, for example, MoleMap New Zealand's mole mapping programme.
The main components are:
- Clinical skin examination and dermatoscopy to identify and evaluate lesions of concern
- Whole body photography
- Close up and dermatoscopic photographs of melanocytic naevi and other skin lesions
- Detection of new or changed lesions at follow-up visits
- Expert dagnosis and management recommendations.
Digital photographic skin surveillance may include:
- Risk evaluation: age, medical and family history, skin typing, sun exposure
- Patient education regarding sun protection, moles, and melanoma
- Skin examination by a trained health professional
- High quality digital images
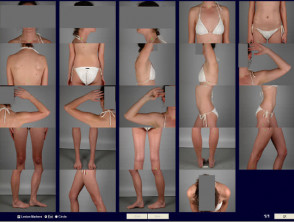
- Standardised poses of the whole body
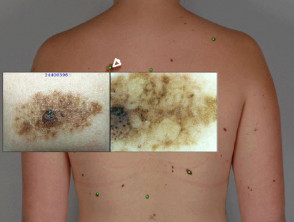
- Close-up macro images of the lesions of concern
- Dermatoscopic images of lesions of concern
- Evaluation of the images by an expert in skin cancer, usually a dermatologist
- A report to the patient and/or referring health practitioner
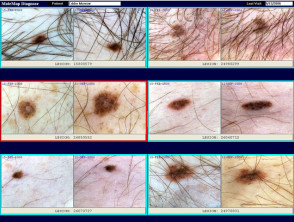
- Follow-up digital dermatoscopic images in 3–6 months (short-term monitoring)
- Follow-up imaging of all imaged lesions at intervals of 1 to 2 years or as recommended by a doctor
- A secure database and transfer system to store the images and reports
- Copies of the images for the patient or doctor to aid in self skin examination.
The patient will be asked to remove at least outer clothing. Make-up, nail varnish and jewellery should be completely removed prior to the procedure. Long hair should be tied up.
Photographic skin surveillance by MoleMap New Zealand
Which lesions should be imaged?
Lesions of concern are those that have features consistent with melanoma or other form of skin cancer (such as basal cell carcinoma or squamous cell carcinoma). Characteristically, skin cancers enlarge or change over periods of weeks to years.
The characteristics of melanoma are defined by the ABCDE rule and the Glasgow 7-point checklist. These are a useful guide, but may not identify early melanomas or atypical forms. Not all skin lesions with these characteristics are melanomas; many turn out to be harmless.
| ABCDE rule | Glasgow 7-point checklist | ||
|---|---|---|---|
| A B C D E |
Asymmetry Border irregularity Colour variation Diameter over 6 mm Evolving (enlarging, changing) |
Major features: Change in size Irregular shape Irregular colour |
Minor features: Diameter >7mm Inflammation Oozing Change in sensation |
Nonmelanoma (or keratinocytic) skin cancers are much more common than melanoma. These usually present as growing skin lesions, that may be crusty, ulcerated or bleeding.
If you have any skin lesions that worry you because they are new, enlarging or look distinctive or unusual, ask your doctor's advice. If your doctor is also concerned, he or she may advise removal (biopsy), follow-up appointment, referral to a specialist, or photographic skin surveillance.
Who should undergo photographic skin surveillance?
Photographic skin surveillance is particularly useful for individuals who have:
- Many moles (more than 50–100)
- Dysplastic or atypical naevi — moles that are large, unusual colour(s) or shapes
- Moles on the back, which may be difficult to keep an eye on
- Previous history of melanoma
- Strong family history of melanoma
- Fair skin that has been severely or repeatedly sunburned
- Concerns about individual moles or freckles, for example because of their appearance or recent change.
Photographic skin surveillance is most useful for pigmented moles – moles that are light to dark brown in colour (rather than pink). Accurate diagnosis depends on evaluation of the structure of the pigment.
What are the advantages of photographic skin surveillance?
Photographic skin surveillance is intended to diagnose melanoma at the earliest possible stage, by identifying new melanocytic lesions or change in pre-existing melanocytic lesions. These features may be suspicious of melanoma if the lesion also has a disordered structure clinically or on dermatoscopy.
Compared to self skin examination or an examination by a non-specialist doctor, photographic skin surveillance has several advantages.
- The previous record can be used to determine whether a lesion of concern is new or has changed.
- If the doctor determines that a lesion has the criteria for removal, this can be done at the earliest possible stage, reducing the risk of melanoma and minimising surgery.
- If a lesion is new or has changed, but does not reach the threshold for removal, it can be re-imaged and watched carefully.
- Lesions that do have not structural disorder and have not changed are very unlikely to be melanoma so may not need to be removed, reducing the potential cost, risks and complications of surgery.
- Digital photographic skin surveillance may be undertaken near where you live, reducing the need to visit a dermatologist at a remote centre.
- Earlier expert evaluation – in many areas there may be a long delay to get an appointment with a dermatologist.
- Reassurance to the patient and their health practitioner(s).
What are the risks of photographic skin surveillance?
Clients should be aware that any screening system has risks.
- There may be a melanoma in a hidden site that has not been imaged, such as the scalp or genitals.
- Early melanoma and other forms of skin cancer may look like a benign skin lesion, and might be missed (false negative).
- A harmless lesion may be misdiagnosed as melanoma, resulting in unnecessary surgery and alarm (false positive).
- Melanoma may grow rapidly, particularly nodular melanoma; it may reach a dangerous size before the next planned visit.
Should I have photographic skin surveillance?
If you are considering undergoing photographic skin surveillance, discuss the procedure with your own doctor. Ensure:
- The procedure includes the elements discussed above.
- You are provided with written information about the procedure, its shortcomings and benefits.
- You and your usual doctor are provided with a report that explains any recommendations for follow-up or treatment of lesions of concern to you, your own doctor or to the skin lesion imaging service.
- If you are concerned about a skin lesion, or you are at high risk of skin cancer, have a full skin examination by a health professional experienced in skin examination and skin cancer detection.