What is pityriasis rubra pilaris?
Pityriasis rubra pilaris (PRP) is the name given to a group of rare skin disorders that present with reddish-orange coloured scaling patches with well-defined borders. They may cover the entire body or just parts of the body such as the elbows and knees, palms and soles.
Often there are areas of uninvolved skin, particularly on the trunk and limbs, which are referred to as islands of sparing.
The palms and soles are usually involved and become diffusely thickened and yellowish (palmoplantar keratoderma). PRP is often initially mistaken for another skin condition, usually psoriasis.
Why does pityriasis rubra pilaris occur and who is at risk?
The cause of PRP is unknown. PRP is usually sporadic but in some forms, it may be partially inherited. It may occur in any race, and males and females are equally affected. It is occasionally precipitated by a drug, such as sorafenib, insulin, imatinib, telaprevir, and vaccinations.
There are several forms of PRP that are classified as follows:
| Type | Features |
|---|---|
| Classical adult-onset |
|
| Atypical adult-onset |
|
| Classical juvenile-onset |
|
| Circumscribed juvenile |
|
| Atypical juvenile-onset |
|
| HIV-associated |
|
What does pityriasis rubra pilaris look like?
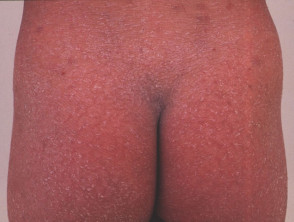
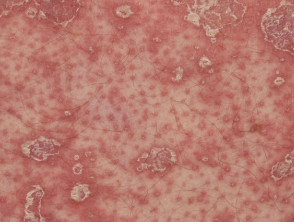
Classical adult-onset PRP
Classical adult-onset PRP most often starts on the head, neck and upper trunk as a red scaly rash. Often there is a solitary lesion but within a few weeks multiple patches appear and they join together to form groups of reddish-orange lesions. Over a few weeks, these spread downwards and may cover most of the body (erythroderma).
Rough, dry plugs can be felt within the patches and are due to plugged hair follicles, often most obvious on the backs of the fingers. Patients may also complain of itching in the early stages of the disease.
The palms and soles become thickened and yellow coloured in PRP. Cracks may develop which can be painful and make walking and using the hands difficult. The nails may become thickened and discoloured at the free nail edge and may show linear black streaks (splinter haemorrhage). The hair may thin considerably.
Adult pityriasis rubra pilaris
Juvenile-onset PRP
PRP in childhood can be classical (generalised) or circumscribed (limited in extent). The appearance is similar to in adults, with prominent thickening of the skin of the palms and soles. Other affected areas can be orange-red in colour with follicular prominence.
Classical juvenile-onset pityriasis rubra pilaris
Circumscribed juvenile-onset pityriasis rubra pilaris
How is pityriasis rubra pilaris diagnosed?
PRP is diagnosed clinically from its time course and clinical appearance, with skin biopsy findings being supportive.
What treatments are available for pityriasis rubra pilaris?
The value of any treatment is difficult to assess, as the clinical course is so variable for each of the different types of PRP. Patients with classical adult onset PRP may present very unwell with acute erythroderma and may require hospital admission for skincare, fluid replacement, and other supportive care.
Topical medications such as emollients and calcipotriol may be used to relieve symptoms of dryness and cracking. Topical corticosteroids are not effective.
Systemic treatments include:
- Methotrexate
- Acitretin
- Isotretinoin
- PRP has been reported to clear with etanercept (TNF-alpha blockade), ustekinumab (IL-12/IL-23 blockade), and secukinumab (IL-17 blockade).
Narrowband ultraviolet (UV)-B phototherapy and extracorporeal photophoresis are also reported as helpful in some patients.
What is the outcome for pityriasis rubra pilaris?
In general, the inherited forms of PRP tend to persist throughout life whilst the sporadically acquired forms tend to resolve spontaneously eventually after one to three years.