Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Author: Hon A/Prof Amanda Oakley, Dermatologist, Hamilton, New Zealand, 1997. Updated by Dr Oakley and Dr Daniela Vanousova, Dermatologist, Czech Republic, in September 2015. DermNet Revision August 2021
Introduction
Demographics
Causes
Clinical features
Complications
Diagnosis
Treatment
Outlook
Molluscum contagiosum is a common viral skin infection of childhood that causes localised clusters of umbilicated epidermal papules.

Pseudo-koebnerisation in a scratch (MC-patient3)
Molluscum contagiosum mainly affects infants and young children under the age of 10 years. It is more prevalent in warm climates than cool ones, and in overcrowded environments. Adolescents and adults are less often infected.
Molluscum contagiosum tends to be more numerous and last longer in children who also have atopic dermatitis, due to deficiencies in the skin barrier. It can be very extensive and troublesome in patients with human immunodeficiency virus (HIV) infection or that have other reasons for poor immune function.
Molluscum contagiosum is caused by a poxvirus, the molluscum contagiosum virus. There are at least 4 viral subtypes.
There are several ways the virus can spread:
Transmission of molluscum contagiosum appears to be more likely in wet conditions, such as when children bathe or swim together. The incubation period is usually about 2 weeks but can be as long as 6 months.
Molluscum contagiosum presents as clusters of small round papules. The papules range in size from 1 to 6 mm and may be white, pink or brown. They often have a waxy, shiny look with a small central pit (this appearance is sometimes described as umbilicated). Each papule contains white cheesy material.
There may be few or hundreds of papules on one individual. They mostly arise in warm moist places, such as the armpit, behind the knees, groin or genital areas. They can arise on the lips or rarely inside the mouth. They do not occur on palms or soles.
When molluscum contagiosum is autoinoculated by scratching, the papules often form a row.
Molluscum contagiosum frequently induces dermatitis around them and affected skin becomes pink, dry and itchy. As the papules resolve, they may become inflamed, crusted, or scabby for a week or two.

Shiny umbilicated papules

Typical umbilicated papules

Associated with eczema
See more images of molluscum contagiosum ...

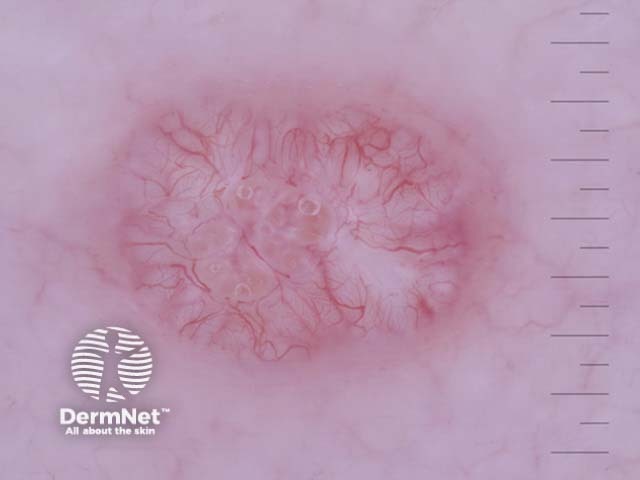
Molluscum contagiosum is usually recognised by its characteristic clinical appearance or on dermatoscopy. White molluscum bodies can often be expressed from the centre of the papules.
Sometimes, the diagnosis is made on skin biopsy. Histopathology shows characteristic intracytoplasmic inclusion bodies.
Molluscum contagiosum

Molluscum contagiosum

Typical rosettes
There is no single perfect treatment of molluscum contagiosum since we are currently unable to kill the virus. In many cases no specific treatment is necessary.
Secondary dermatitis may be treated symptomatically with a mild topical topical corticosteroid such as hydrocortisone cream. Dermatitis is unlikely to fully resolve until the molluscum infection has cleared up.
Molluscum contagiosum is infectious while active. However, affected children and adults should continue to attend daycare, school, and work.
To reduce spread:
In immune competent hosts, molluscum contagiosum is a relatively harmless. The papules may persist for up to 2 years or longer. In children, about half of cases have cleared by 12 months, and two-thirds by 18 months, with or without treatment. Contact with another infected individual later on can lead to a new crop.
Infection can be very persistent in the presence of significant immune deficiency.