DermNet provides Google Translate, a free machine translation service. Note that this may not provide an exact translation in all languages
Home Dermatopathology Preparation of specimen CME
Dermatopathology
Preparation of specimen
Learning objectives
- Describe the preparation of a skin specimen for histopathology
- Explain potential errors in pathological diagnosis
Introduction
Skin biopsies are taken for the following reasons:
- To make or confirm a clinical diagnosis
- To remove a skin lesion
- Research
Dermatopathology is necessary to make or confirm a clinical diagnosis and determine whether margins of excision are adequate.
After a piece of skin is removed the specimen is sent ta surgical pathology (histology) laboratory. A general histopathologist or a specialist dermatopathologist examines processed routine sections under a light microscope. In some cases, special stains or other tests are required for diagnosis. A report is then issued to the referring practitioner.
Skin biopsy specimens
Specimens of skin removed for pathological examination ideally should contain a representative sample of epidermis, dermis and subcutaneous tissue. The skin biopsy may be one of the following types: :
| Excision biopsy | A skin lesion is completely cut out for diagnosis and treatment |
| Incisional biopsy | A segment of the lesion is removed for diagnosis only |
| Shave / tangential biopsy | A horizontal section of the skin is removed for diagnosis or treatment |
| Punch biopsy | A standard round specimen 2-6 mm in diameter for diagnosis |
| Currettings | Fragments of tissue are removed using a ring or spoon curette for treatment |
| Fine Needle Aspiration | A needle is inserted into the lesion and cells are aspirated for direct examination. |
The sample should be transported in fixative (usually 10% neutral buffered formalin); the volume should be at least ten times that of the tissue. Make sure the pot is properly sealed. Label it with the patient's full name and a second identifier (date of birth and/or National Health Index number), the site of the biopsy and the date.
A request form should accompany specimens to the pathology laboratory. The form should include patient details including age and sex, a description of the specimen type, the exact site of the biopsy, and clinical details including as a minimum the suspected diagnosis, differential diagnosis and brief clinical history, including duration of the lesion and any treatment applied.
In the laboratory
Fixation
The purpose of fixation is to preserve the skin specimen indefinitely in a life-like state. For normal histological sections, the specimen of skin is immediately placed in formol saline (formalin). It remains in this preservative for a minimum of 24 hours prior to processing by a histotechnologist.
Formalin fixes the tissue by forming cross-links between lysine residues in the proteins, which does not alter their structure. It is buffered with phosphate to prevent acidity provoked by tissue hypoxia, maintaining a pH of 7. It penetrates effectively into the tissue but rather slowly, depending on its thickness; tissues can be fixed faster if they are warmed.
If no fixative is available at the time of biopsy, the specimen should be kept moist with saline and transported to the laboratory as soon as possible; contact the lab in advance to confirm that there will be someone available to receive it.
Tissue processing
The technologist assigns the specimen a unique accession number, examines it and describes the gross appearance of the specimen. If malignancy is suspected, the edges of the specimen may be marked with ink to identify excision margins. All or parts of the specimen are placed into one or more small plastic cassettes which hold and identify the tissue while it is being processed, and which acts as the backing for the final paraffin block. Initially, the cassettes are placed into a fixative.
Paraffin blocks are then prepared to allow the tissue to be cut into thin microscopic sections (3–5 microns). Using an automated processor, the water is removed from the tissue by alcohol dehydration. The alcohol is cleared using xylene and then the tissue is ready to be embedded in paraffin wax. The technician removes the tissue from its cassette, aligns it carefully in a mould and pours hot paraffin wax over it. As the wax cools, it solidifies to form the block ready for sectioning.
Large laboratories may use a microwave processing machine when tissue needs to be processed rapidly, eg, within 2 hours, but these are not generally available.
Sectioning
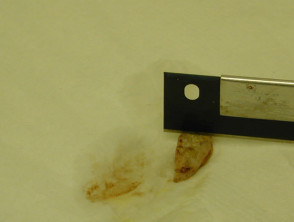
The embedded tissue is cut into sections using a microtome, which moves the block across a very sharp knife every 3 to 5 microns. The sections are then floated on a warm water bath, picked up on a glass microscope slide and dried in a warm oven.
Preparation of the specimen
Staining
By another automated process, the paraffin is removed from the sections by sequentially immersing in xylene, then alcohol and then water. The slide is then stained routinely using haematoxylin and eosin (H and E). This is an automated process in larger laboratories, but some centres stain manually. In some situations, other special stains may be used.
- Haematoxylin stains include a variety of metal cations that result in varying hues (blue). It is a basic dye that stains the nucleic acids of the cell nucleus and is usually partially removed by an acid-alcohol solution.
- Eosin stains are acidic and dye cytoplasmic components of the cell red.
Mounting
The stained slide is processed again through water, alcohol and xylene. A resin is applied to glue a coverslip or plastic film in place over the section. The slide is now ready for the pathologist to examine and report the microscopic description, the diagnosis and comments.
Potential errors
If the tissue is not processed carefully, various artefacts may be present on the slide.
| Fine black spots | Formalin-haem pigment if the formalin used is too acidic (unbuffered). |
| Holes | Tearing by microtome because of insufficient tissue dehydration or the presence of hard material such as calcium or sutures. |
| Bubbles | Mounting media to thin or contaminated clearing agents. |
| Carryover artefacts and floaters | Tissue from another specimen is carried over on the sectioning knife or has dropped onto the slide in the water bath because of inadequately cleaning between cases |
Mislabelling specimens or lack of labelling is another potential error, although blocks are usually routinely given two means of identification (eg, name and lab number) to prevent this.
Laboratory safety
- The chemicals used in tissue processing are potentially toxic.
- The laboratory should have good ventilation.
- Chemicals must be correctly labelled and stored.
- A materials safety data sheet should be available.
- Hazardous wastes must be safely disposed of.
- Occupational hazards should be identified and every precaution taken to reduce danger.
Activity
Arrange to visit your local medical laboratory and ask to be shown the techniques described above.
Related information
On DermNet NZ
Information for patients
Other websites
- Breadloafing a skin specimen. Dr Ian Katz. Youtube.
- Florida State University WebPath Histotechniques – Anatomy histology tutorials
Books about skin diseases
Sign up to the newsletter
© 2024 DermNet.
DermNet does not provide an online consultation service. If you have any concerns with your skin or its treatment, see a dermatologist for advice.