DermNet provides Google Translate, a free machine translation service. Note that this may not provide an exact translation in all languages
Home Dermatological emergencies Erythroderma CME
Dermatological emergencies
Erythroderma
Created 2008.
Learning objectives
- Identify the causes of erythroderma, its complications and management principles
Clinical features
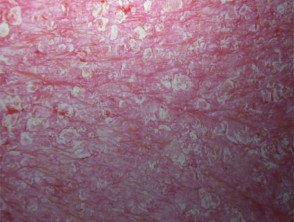
Erythroderma is the term used to describe inflammatory skin disease affecting the entire skin surface. It may be acute or chronic. It often precedes or is associated with exfoliation when it may also be known as exfoliative dermatitis.
Causes include:
- Adverse drug eruption (most often sulphonamides, penicillin, antimalarials, anticonvulsants and allopurinol)
- Dermatitis (any kind)
- Psoriasis
- Pityriasis rubra pilaris (PRP)
- Immunobullous disease
- Cutaneous T-cell lymphoma (Sézary syndrome)
- Underlying systemic malignancy
- Graft vs Host disease
- HIV infection
Erythroderma
Clinical features depend on the underlying cause. Generalised skin redness (erythema) may be accompanied by oedema (especially if due to eczema or drugs), serous exudate (eczema), scaling (eczema, psoriasis). Degree of itch varies from none (PRP) to intolerable (eczema, bullous diseases). Other features include:
- Hair loss
- Keratoderma of palms and soles
- Nail shedding or nail dystrophy
- Ectropion
- Hyper- or hypopigmentation
- Localised or generalised lymphadenopathy
Complications may include:
- Secondary infection
- Loss of temperature control
- High output heart failure
- Fluid and electrolyte imbalance
- Hypoalbuminaemia
Investigations
Investigations should be performed to identify underlying causes and complications. They may include:
- Skin swabs for bacterial culture
- Haematology and biochemistry
- Skin biopsy (results depend on underlying cause)
Management
The underlying cause of erythroderma should be established if possible. Most patients with acute erythroderma require hospitalisation to restore fluid and electrolyte balance, circulatory status and body temperature. However, erythroderma may also be relatively asymptomatic and managed as outpatient.
- Discontinue all unnecessary medications
- Apply emollients and mild topical steroids
Where relevant:
- Wet dressings
- Manage fluid balance and body temperature
- Oral or intravenous antibiotics
- Sedative antihistamines
Systemic treatment depends on the underlying cause and should be directed by a dermatologist.
Activity
Compare erythroderma arising in childhood with that occurring in the elderly.
Related information
On DermNet NZ:
Information for patients
Other websites:
- Medscape Reference: Erythroderma (Generalized Exfoliatve Dermatitis)
- Merck Medicus Best Practice of Medicine: Generalised rash
Books about skin diseases:
See the DermNet NZ bookstore
Sign up to the newsletter
© 2024 DermNet.
DermNet does not provide an online consultation service. If you have any concerns with your skin or its treatment, see a dermatologist for advice.