DermNet provides Google Translate, a free machine translation service. Note that this may not provide an exact translation in all languages
Home Follicular disorders Acne CME
Follicular disorders
Acne
Created 2009.
Learning objectives
- Recognise acne variants
- Manage a straightforward case of acne
Introduction
Acne is a follicular disorder that mainly affects adolescents but may persist or even become more severe in adulthood. Most, but not all, acne patients have oily skin (seborrhoea).
Usually several types of acne spots appear on the face, but they also may arise on the chest, back and sometimes even more extensively.
Non-inflammatory lesions:
- Open comedones (blackheads)
- Closed comedones (whiteheads)
- Cysts
Non-inflammatory acne lesions
Inflammatory lesions:
- Papules
- Pustules
- Inflammatory nodules
Inflammatory lesions
Secondary lesions:
- Excoriations
- Postinflammatory erythematous macules (in fair skin)
- Postinflammatory pigmented macules (in dark skin)
- Scars (atrophic, hypertrophic or ice-pick)
Secondary lesions
Pathophysiology of acne
The primary lesion of acne is the comedone, a follicular plug of sebum and keratin.
Sebum
Sebaceous glands are larger and most numerous on the acne-prone sites i.e. mid-back, forehead and chin. They are also numerous in the ear canal and around the genitals.
Sebum is a complex and variable mixture of lipids including:
- Glycerides
- Free fatty acids
- Wax esters
- Squalene
- Cholesterol esters
- Cholesterol
Triglycerides produced by sebaceous glands are broken down by bacterial lipases in the sebaceous duct to form free fatty acids.
Sebum has the following functions:
- It reduces water loss from the skin surface;
- It protects the skin from infection by bacteria and fungi;
- It contributes to body odour;
- It is colonised by bacteria especially Proprionibacterium acnes.
Sebaceous gland cells are stimulated to produce more sebum by androgens. Type 1 5-a reductase in the skin converts less active androgens into testosterone and 5-a testosterone (DHT).
In a fetus, the sebaceous product is a waxy protective layer, vernix caseosa. For 3 to 6 months after birth, sebum resembles that of an adult then it reduces in amount and wax content until the inevitable rise at puberty. In females, oil production is slightly greater in the second half of the menstrual cycle. After the mid-20's, sebum production declines, particularly after the menopause in females.
Pituitary, adrenal, ovarian or testicular disorders may increase or reduce sebum;
- Parkinson disease increases it;
- Prolonged starvation reduces it;
- Oestrogens, antiandrogens and retinoids reduce it;
- Testosterone, medroxyprogesterone, levonorgestrel and phenothiazines increase it.
Inflammation
Inflammatory mediators include:
- IL-1a, IL-b and TNF released by sebaceous duct cells;
- Bacterial lipases. proteases, hyaluronate lyase, phosphatase, smooth-muscle contracting substances and chemoattractants to polymorphonucleocytes and monocytes.
Rupture of the duct causes a foreign body granulomatous reaction and releases free fatty acids and sebum into the dermis.
Comedonal acne
Comedones often arise on the forehead and chin. Comedonal acne may be aggravated by:
- Hormonal factors
- Humid weather
- Oily cosmetics such as pomades, sunscreens and petroleum-based moisturisers.
Management
- Use oil-free cosmetics
- Wash twice daily with a mild soap or cleanser and water.
- Topical comedolytic agents applied once or twice daily as a thin smear to the entire area
- Hormonal therapy (females)
It may take several months for significant improvement. Suitable topical agents include:
- Benzoyl peroxide 2.5-10%
- Azelaic acid 20%
- Salicylic acid +/- sulphur +/- resorcinol 1-3%
- Glycolic acid 10-20%
- Topical retinoid (tretinoin, isotretinoin, adapalene): requires prescription
Comedonal acne
Antibiotics are not usually very effective for this pattern of acne. Persistent or unresponsive comedonal acne warrants referral to a dermatologist for oral isotretinoin. Comedones may also be removed by electrosurgery or microdermabrasion.
Acne vulgaris
Acne vulgaris refers to the common presentation of comedones and superficial inflammatory lesions (papules and pustules). Individual spots last up to two or three weeks.
Acne may be considered mild, moderate or severe. Comedones and inflammatory lesions are usually considered separately. The more complex Leeds' grading scale (1 to 12) compares inflammatory lesions with standard photographs.
Acne vulgaris
Acne severity depends on:
- Genetic factors;
- Hormonal factors e.g. polycystic ovaries, corticosteroids (most often exogenous);
- Presence of psychological stress and depression;
- Environmental factors including high humidity, occlusive cosmetics and clothing;
- Medications that affect sebum production.
Despite popular belief, dietary factors are rarely important. High dairy intake may affect some individuals, possibly because of the hormones found in milk. High glycaemic index foods have also been blamed. The evidence is weak.
Management
Mild acne vulgaris should be treated with topical agents (see comedonal acne). Topical antibiotics may be added but should not be used alone because of the risk of inducing resistant organisms. Twice weekly blue light treatment may also be helpful.
Moderate acne vulgaris should be treated with topical comedolytic agents and anti-inflammatory oral antibiotics (tetracycline or one of its derivatives, or a macrolide). Reduce the risk of inducing P. acnes antibiotic resistance; address compliance issues, and combine with topical keratolytics. Do not use topical antibiotics at the same time as oral antibiotics. There is rarely benefit from switching from one antibiotic to another; the chosen drug may be required for 6 months or longer.
In females with no history of or risk factors for thromboembolic disease, the combined oral contraceptive pill is useful, especially those containing progesterones with minimal androgen effect or that are antiandrogenic. Where oestrogens are contraindicated, spironolactone or low dose corticosteroids may be warranted particularly if there is adrenal hyperandrogenism.
Ethinyl oestrodiol / cyproterone acetate can be used for polycystic ovarian syndrome and resistant acne but compared with other so-called second generation pills may have an increased risk of thromboembolic disease. Newer antiandrogenic progesterones such as drospirinone or denogest do not appear to have this increased risk.
Oral isotretinoin should be considered for patients with long-standing acne, acne that resists treatment or recurs rapidly on discontinuing effective treatment. In New Zealand, oral isotretinoin requires Special Authority application for funding by PHARMAC, and restrictions apply.
Infantile acne
Infantile acne generally affects the cheeks, and sometimes the forehead and chin of newborn babies. It is more common in boys and is usually mild. In most children it settles down within a few months but they may develop troublesome acne at puberty. The cause is thought to be fetal hormones.
Infantile acne
Neonatal cephalic pustulosis (previously known as ‘neonatal acne’) is due to malassezia proliferation. Tiny papules and pustules erupt on the face and upper trunk of healthy young babies. The lesions persist for days to weeks and generally resolve without treatment. There are no comedones.
Management
Treatment is usually with topical agents such as benzoyl peroxide or erythromycin gel. Sometimes, oral erythromycin or isotretinoin may be required. NOTE: tetracycline antibiotics should not used because they may cause yellow staining of the developing permanent teeth.
Nodulocystic acne
Nodulocystic acne is a severe form of acne affecting the face, chest and back. It is characterised by multiple inflamed and uninflamed nodules and scarring. It is called acne conglobata when there are draining sinuses. It is more common in males. It is known as acne conglobata when there are interconnected abscesses and sinuses; these can cause very severe hypertrophic and atrophic scars.
Nodulocystic acne
Management
Patients with nodulocystic acne should consult a dermatologist as management may be tricky. While waiting to be seen, they should receive an oral antibiotic. The recommended treatment is oral isotretinoin, which should be commenced early to prevent scarring. The treatment is required for at least five months, and further courses are sometimes necessary.
When isotretinoin is unavailable or unsuitable, systemic antibiotics, and in women, hormonal therapy, may also be helpful. Topical treatment is usually ineffective for the nodules but topical retinoid and topical benzoyl peroxide should be prescribed for the superficial lesions. Individual cysts may shrink with intralesional injections with 2mg triamcinolone acetonide.
Acne fulminans
Acne fulminans is a rare and very severe form of acne conglobata associated with systemic symptoms. It nearly always affects males. It is characterised by:
- Abrupt onset
- Inflammatory and ulcerated nodular acne on chest and back
- Severe acne scarring
- Fluctuating fever
- Painful joints
- Malaise
- Loss of appetite and weight loss
- Raised white blood cell count.
It is thought to be due to hypersensitivity to P. acnes. Although it mostly just happens, it may be precipitated by:
- Testosterone (legal or illegal)
- Isotretinoin
Acne fulminans
Management
Patients with acne fulminans should consult a dermatologist urgently. Management can prove difficult, and several medications are usually required. These may include:
- High doses of oral antibiotics such as erythromycin (2g/day)
- Anti-inflammatory medications such as salicylates (aspirin)
- Prednisone (20-60mg/day)
- Dapsone
- Isotretinoin
Topical acne medications are unhelpful.
Hidradenitis suppurativa
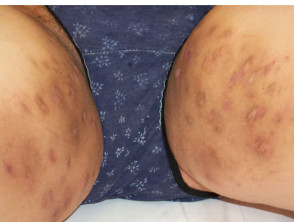
Hidradenitis is another form of follicular occlusion syndrome that affects axillae and groins primarily, with submammary and buttock areas involved in some cases. The role of inflamed apocrine glands is uncertain. The result is tender nodules, fluctuant cysts, discharging abscesses, sinuses and scarring. It is associated with nodulocystic acne and pilonidal sinus.
Hidradenitis suppurativa
Management
Hidradenitis is fairly resistant to treatment. Currently, 3-month courses of clindamycin and rifampicin are favoured (require specialist approval for Drug Tariff subsidy in New Zealand). The following may also be beneficial:
- Short courses of anti-staphylococcal antibiotics for acute flare-ups
- Longer courses of tetracycline antibiotics (3 to 6 months) for their anti-inflammatory action
- Anti-androgenic hormones for females
- Isotretinoin or acitretin for 6 to 12 months
- Surgical drainage of abscesses or widespread excision of apocrine gland-bearing skin
Activity
Discuss the use of contraceptive agents for acne patients taking isotretinoin.
Related information
On DermNet NZ:
Information for patients
Other websites:
- Medscape Reference: Diseases of the adnexa
- Medscape: Adolescent Acne: A Stepwise Approach to Management from Topics in Advanced Practice Nursing eJournal, April 2002
- WHO: Medical eligibility criteria for contraceptive use
- Arowojolu AO, Gallo MF, Grimes DA, Garner SE. Combined oral contraceptive pills for treatment of acne. Cochrane Database Syst Rev. 2005;(3):CD004425. Review. Medline
- Medsafe Prescriber Update: Ministry of Health (Medsafe) advice on the use of combined oral contraceptives
- Gollnick H, Cunliffe W, Berson D, Dreno B, Finlay A, Leyden JJ, Shalita AR, Thiboutot D. Management of acne: a report from a Global Alliance to Improve Outcomes in Acne. J Am Acad Dermatol. 2003 Jul;49(1 Suppl):S1-37. Review. Medline
- Merck Manual Professional: Acne Vulgaris
Books about skin diseases:
See the DermNet NZ bookstore
Sign up to the newsletter
© 2024 DermNet.
DermNet does not provide an online consultation service. If you have any concerns with your skin or its treatment, see a dermatologist for advice.