What is contact urticaria?
Contact urticaria is an immediate but transient localised swelling and redness that occurs on the skin after direct contact with an offending substance. Contact urticaria should be distinguished from contact dermatitis where a dermatitis reaction develops hours to days after contact with the offending agent.
Contact urticaria can be immunological (due to allergy) or non-immunological. It is a form of inducible urticaria and can be acute or chronic.
Contact urticaria
Who gets contact urticaria?
Anyone is able to get contact urticaria, however, there are some groups of people that are at increased risk for the condition to occur. Occupational groups at risk and the substances that cause contact urticaria are listed below. In most cases, exposure has occurred over time and the response is of the immunological type of contact urticaria.
- Agricultural and dairy workers: cow dander, grains and feeds
- Bakers: ammonia persulfate, flour, alpha-amylase
- Dental workers: latex, acrylate and epoxy resins, toothpaste
- Electronic workers: acrylate and latex
- Food workers: foodstuffs, such as cheese, egg, milk, fish, shellfish, fruit, flour, wheat
- Hairdressers: ammonia persulfate, latex
- Medical/veterinary workers: latex
What causes contact urticaria?
Contact urticaria is caused by a variety of compounds, such as foods, preservatives, fragrances, plant and animal products, metals, and rubber latex. The mechanism by which these provoke an immediate urticarial rash at the area of contact can be divided into two categories: non-immunological contact urticaria and immunological (allergic) contact urticaria.
- Non-immunological contact urticaria typically causes mild localised reactions that clear within hours, for example, stinging nettle rash. This type of urticaria occurs without prior exposure to a patient's immune system to an allergen.
- Immunological contact urticaria occurs most commonly in atopic individuals (people who are prone to allergy). Hence prior exposure to an allergen is required for this type of contact urticaria to occur.
Commonly reported causes of the different types of contact urticaria are shown below.
Non-immunological contact urticaria
- Ingredients of cosmetics and medicaments
- Balsam of Peru
- Benzoic acid
- Cinnamic alcohol
- Cinnamic aldehyde
- Sorbic acid, a commonly used preservative in many foods
- Raw meat, fish, and vegetables
Immunological contact urticaria
- Natural rubber latex (e.g. surgical gloves)
- Many antibiotics
- Some metal, e.g. nickel
- Parabens
- Benzoic and salicylic acids
- Polyethylene glycol
- Short chain alcohols
- Raw meat, fish, and vegetables
What are the clinical features of contact urticaria?
Contact urticaria reactions appear within minutes to about one hour after exposure of the offending substance to the skin. Signs and symptoms of affected skin areas include:
- Local burning sensation, tingling or itching
- Localised or generalised red swellings or weals may occur, especially on the hands. The severity of redness and swelling can range from slight redness or spots with minimal swelling to fiery redness with tense swelling and weals.
- Rash usually resolves by itself within 24 hours of onset.
Signs and symptoms may occur in other organs other than the skin. These are known as extracutaneous reactions and are more likely to occur in patients with immunological contact urticaria. Features of extracutaneous reactions include:
- Wheezing (bronchial asthma)
- A runny nose, watery eyes
- Lip swelling, hoarse throat, difficulty swallowing
- Nausea, vomiting, diarrhoea, cramps
- Severe anaphylactic shock (this can be life-threatening)
Contact urticaria
How is contact urticaria diagnosed?
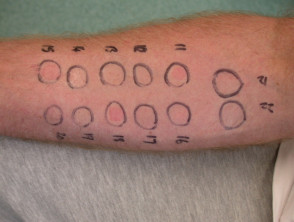
Sometimes it is easy to recognise contact urticaria and no specific tests are necessary. RAST tests (specific IgE blood test) where available, can be used to confirm the allergy. Skin prick test and scratch patch tests confirm the diagnosis of contact urticaria but do not differentiate between allergic and non-allergic mechanisms.
What is the treatment for contact urticaria?
The patient should have an understanding of the nature of their urticarial reaction (non-immunological vs immunological). Patients with immunological contact urticaria should wear medical alert tags and be aware of the potential life-threatening reactions of the condition.
In most cases, the rash rapidly clears up completely once the offending substance is no longer in contact with the skin.
The main aim of treatment is to avoid the substances that cause the urticarial reaction and find suitable alternatives. Gloves may be used to protect hands from contact with materials of concern, but avoid rubber gloves if allergic to latex.
Medications that may be used to minimise the reaction include antihistamines and adrenaline for more severe reactions.