What is vaginitis?
The term 'vaginitis' means an inflamed vagina; the term is loosely used to refer to any vaginal condition that results in a vaginal discharge, whether due to infectious or non-infectious causes.
What is aerobic vaginitis?
Aerobic vaginitis is characterised by:
- Vaginal inflammation
- Atrophy of vaginal epithelium
- Abnormal vaginal microflora including:
- Increased levels of aerobic bacteria
- Decreased levels of lactobacilli.
Aerobic vaginitis was first characterised by Donders et al in 2002. Desquamative inflammatory vaginitis is a severe form of aerobic vaginitis [1,2].
Who gets aerobic vaginitis?
Aerobic vaginitis may affect adult women of any age, whether pre- or post-menopause. The prevalence of aerobic vaginitis has been estimated in different populations as being present in 5–13% of asymptomatic women and affecting a greater proportion of women with vaginal symptoms. It may be less prevalent among pregnant women.
The risk factors for infection are under evaluation.
What is the cause of aerobic vaginitis?
The cause of aerobic vaginitis is unknown. Aerobic vaginitis is a form of dysbiosis, a disturbance in the ecology of aerobic micro-organisms that reside in the vaginal microflora (the microbiome). These microorganisms include:
- Escherichia coli
- Staphylococcus aureus
- Coagulase-negative staphylococci (eg, S. epidermidis)
- Streptococcus agalactiae
- Enterococcus faecalis.
It is unclear whether the primary cause of aerobic vaginitis is pathogenic organisms, lack of lactobacilli, immune dysregulation and pro-inflammatory cytokines, or insufficient oestrogen in the vaginal mucosa (atrophic vulvovaginitis) [2].
What are the clinical features of aerobic vaginitis?
The symptoms of aerobic vaginitis can fluctuate over a long period of time. They include [2]:
- Vaginal stinging and burning sensations
- Dyspareunia
- A sticky yellow or green discharge with a rotten odour.
Examination findings may include:
- Vaginal inflammation (introital and vaginal redness, oedema, and sometimes, petechiae and ecchymoses)
- Vaginal epithelial disruption (erosions and ulcers)
- Increased vaginal pH.
What are the complications of aerobic vaginitis?
Aerobic vaginitis has been associated with [2]:
- Other forms of vaginitis
- Infection-related miscarriage, premature rupture of membranes, ascending chorioamniotis (inflammation around the fetus), and preterm birth
- Activation of human papillomavirus infection and cervical cancer, possibly due to increased pH and lack of lactobacilli
- Increased risk of acquiring sexually transmitted infections, due to erosions in vaginal mucosa
- Pelvic inflammatory disease and infertility [4].
How is aerobic vaginitis diagnosed?
The diagnosis of aerobic vaginitis is confirmed by wet–mount microscopy of fresh vaginal fluid, ideally using phase contrast. The aerobic vaginitis score is graded as 0–3 (absent), 3–4 (mild), 5–6 (moderate), and 6–10 (severe). The aerobic vaginitis score is calculated from the [1]:
- Lactobacillary grade (LBG): I–III, namely, (I) numerous pleomorphic lactobacilli, with no other bacteria; (IIa) mixed flora, but predominantly lactobacilli; (IIb) mixed flora, but proportion of lactobacilli severely decreased due to increased numbers of other bacteria; and (III) lactobacilli severely depressed or absent because of overgrowth of other bacteria
- Number of leucocytes compared to epithelial cells
- Proportion of toxic leucocytes (these are recognised by their cytoplasmic granules)
- Characteristics of the microflora (eg, cocci and coliforms)
- Presence of immature or parabasal epithelial cells (the cells most typically seen on a vaginal smear).
Vaginal cultures are useful only for clinical research and to detect group A streptococci, trichomoniasis, and Candida albicans infection.
Various advanced diagnostic methods are being established for aerobic vaginitis.
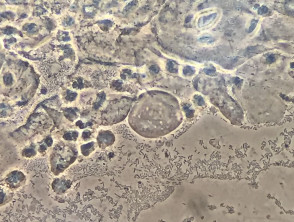
Phase contrast microscopy of aerobic vaginitis
*Credit: Pedro Vieira Baptista
What is the differential diagnosis for aerobic vaginitis?
Aerobic vaginitis is distinct from other forms of infectious vaginitis — particularly bacterial vaginosis, with which it is often confused. The characteristics of bacterial vaginosis are:
- A lack of symptoms
- Greyish-white, watery vaginal discharge with fishy odour
- A lack of inflammation on vaginal examination
- Microscopy findings of decreased lactobacilli and granular flora.
What is the treatment for aerobic vaginitis?
The treatment of aerobic vaginitis depends on the microscopic findings and patient needs [2].
- Topical corticosteroids (eg, hydrocortisone cream or foam) are used to treat a prominent inflammatory component (ie, > 20 leucocytes per epithelial cell on microscopy).
- Antimicrobials (topical, oral or suppository) are used to eradicate pathogenic bacteria; these can include:
- An antiseptic (eg, dequalinium chloride)
- Topical antibiotic (eg, topical kanamycin or clindamycin; note clindamycin can promote bacterial resistance)
- An oral antibiotic (eg, amoxicillin–clavulanic acid or moxifloxacin).
- Topical oestrogen is used to treat vaginal atrophy (ie, when parabasal cells are > 10% of epithelial cells on microscopy).
- Vaginal probiotics are used to restore vaginal lactobacilli.
Metronidazole, which is used for bacterial vaginosis, and antifungal agents, used for Candida albicans infection, are not effective in aerobic vaginitis.
Expert advice should be sought from a medical microbiologist in pregnant women with aerobic vaginitis.