What are pressure ulcers?
Pressure ulcers are skin and soft tissue injuries sustained from prolonged pressure. Specifically, they involve a breakdown of the skin, subcutaneous tissues and sometimes even deeper structures (tendons, muscle, bone) caused by cumulative pressure and are often related to pre-existing health conditions or injuries.
Pressure ulcers are also known as pressure sores, decubitus ulcers, or bed sores. They are often found on bony areas of the body with a thin soft tissue covering.
Who gets pressure ulcers?
Although pressure ulcers can affect anyone, they are most often seen in the elderly and critically ill who are immobile for long periods.
High-risk groups include palliative care patients, comatose patients, quadriplegics, patients with spinal cord injuries, elderly people with orthopaedic fractures, and children with neurological dysfunction (eg, spina bifida, cerebral palsy, or spinal cord injury).
Pressure ulcers carry a high economic and psychological burden, due to hospital admissions for treatment of pressure ulcer complications and reduced quality of life for affected patients.
What causes pressure ulcers?
The most important cause of pressure ulcers is external pressure at a skin site for prolonged periods, although the exact mechanism is complex and poorly understood.
A proposed mechanism involves a complex interplay of local tissue ischaemia, reperfusion injury, increased capillary permeability, increased autophagy, and cell senescence causing direct insult to skin cells. After the inciting external pressure is gone, patients have a delayed reperfusion time which increases the risk of ulcer formation.
A ‘prolonged inflammatory phase’ hypothesis has also been proposed, whereby pressure ulcers do not follow the normal trajectory of inflammation, remodelling, and maturation, but are instead arrested in the ‘inflammatory’ phase of wound healing.
Identifying external and internal risk factors is important to prevent or minimise pressure ulcers.
External factors include:
- Trauma to the skin (eg, skin tears from dressings, lacerations)
- Amputations
- Physical restraints or chemical sedation, worsening immobility
- Inadequate changes in the positioning of immobile patients
- Ill-fitted medical devices (eg, Jewett braces, orogastric and nasogastric tubes, tracheostomy tubes, prosthetics, casts, and splints).
Internal factors include:
- Neurological diseases (both motor and sensory)
- Metabolic syndromes (eg, obesity, diabetes mellitus)
- Cardiovascular disease
- Peripheral arterial occlusive disease
- Malnutrition
- Advanced age.
What are the clinical features of pressure ulcers?
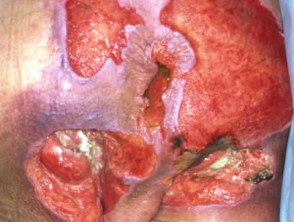
The clinical features of pressure ulcers range from inflamed-looking, to severely ulcerated skin exposing muscle, tendon, and even bone. Commonly affected sites include the skin overlying the coccyx, vertebral column, heels, ankles, and elbows.
For patients who spend prolonged periods lying on their side, the iliac crest, the trochanters, and the ear helix may be affected. During the prolonged prone nursing of patients with severe COVID-induced respiratory disease, facial pressure ulcers were frequent.
The revised National Pressure Ulcer Advisory Panel’s (NPUAP) Pressure Injury Staging System is widely used in the staging and severity assessment of pressure ulcers based on their clinical features.
Other scoring systems, such as the Braden scale, are also used in some healthcare institutions.
Stage 1 pressure ulcers
- Intact skin with various degrees of erythema that does not blanch (turn white) when compressed.
- Skin may be tender, itchy, or painful.
Stage 2 pressure ulcers
- Skin is red, swollen, and painful.
- Partial-thickness skin loss involving a break in the dermis.
- Ulcers appear shiny or dry with a red-pink wound bed with serum-filled blisters.
- Upper layers of skin begin to die.
- Adipose tissue, granulation tissue, slough, and eschar are absent.
Stage 3 pressure ulcers
- Full-thickness skin loss involving the hypodermis.
- Crater-like ulceration is present.
- Adipose tissue may be seen but not muscle, tendon, ligament, cartilage, or bone.
- The depth of tissue damage varies by anatomical location (eg, may appear shallow in low adiposity areas such as occiput and malleolus, while high adiposity areas like the gluteal area may appear deep).
- Wounds are prone to infection.
Stage 4 pressure ulcers
- Full thickness with exposed muscle, tendon, ligament, cartilage, joint, or bone.
- Blackened dead tissue called eschar may be seen in deep open wounds.
- The risk of osteomyelitis is extremely high.
How are pressure ulcers diagnosed?
Pressure ulcers remain a clinical diagnosis. The patient’s skin should be examined thoroughly from scalp to toe. Special attention must be given to skin in common pressure sites, under medical devices, and skin folds in patients with larger body habitus.
The mnemonic ‘BEST SHOT’ is used by the NHS Stop the Pressure campaign as a checklist for common pressure ulcer sites:
- Buttocks
- Elbows and ears
- Sacral area
- Trochanters
- Spine and shoulders
- Heels
- Occiput
- Toes.
Temperature sensing technologies such as infrared thermography (IRT) have been developed to aid early prediction and early diagnosis of pressure ulcers. In a blinded prospective study of 70 patients in an ICU, IRT was found to detect skin changes 5–18 days before the visible appearance of pressure ulcers.
How do clinical features vary in differing types of skin?
Stage 1 pressure ulcers may be missed in darker skin types (eg, Fitzpatrick type 4–6) due to the absence of visible blanching or erythema.
Other parameters such as altered skin sensation, warmth, and skin firmness should be assessed in patients with darker skin types.
What are the complications of pressure ulcers?
- Infection (cellulitis, abscess, osteomyelitis, septic arthritis, necrotising fasciitis, sepsis)
- Malignant transformation
- Ulcer recurrence
What is the differential diagnosis for pressure ulcers?
- Superficial friction injuries or excoriations
- Thermal burns
- Cellulitis
- Marjolin ulcer
- Martorell ulcer
- Vasculitides eg, cutaneous vasculitis
- Radiation injuries eg, radiation dermatitis
- Delayed pressure urticaria
- Diabetic foot ulcers
- Leg ulcers eg, stasis ulcer, arterial ulcer
- Pyoderma gangrenosum.
What is the treatment for pressure ulcers?
General measures
- Alleviate external factors eg, cleanse and dry skin after incontinence, and use barrier creams and emollients.
- Special dressings and honey preparations may be used to help the healing process.
- Dead tissue may be removed with a scalpel (debridement).
- Improve internal factors eg, patient nutrition.
- Optimise the wound bed for maximal healing.
- Minimise pressure on the affected area by turning and pressure relieving devices (cushions, mattresses).
Specific measures
- Occlusive wound dressings to maintain a moist wound environment.
- Regular patient and wound care reviews by a multidisciplinary team (may involve endocrinologists, neurologists, geriatricians, wound care nurses, infectious disease specialists, podiatrists, dietitians, and occupational therapists).
- Negative pressure dressings for severe pressure ulcers.
- Sometimes maggot debridement therapy is used to remove necrotic material and eschar.
- Hydrotherapy debridement, using saline solution in a syringe or a water pressure jet.
- Antibiotics if required for infection.
- Healthy skin may be grafted onto the damaged area.
- Bioengineered skin is also an emerging alternative therapy for skin grafting.
- In severe or life-threatening situations, amputation of a limb may be necessary.
How do you prevent pressure ulcers?
Prevention of pressure ulcers can be classified into 3 domains: promoting movement, pressure reduction, and pressure distribution.
Prevention strategies include:
- Meticulous skin care eg, emollients, gentle cleansers, and avoiding friction and shearing forces
- Optimising patient nutrition and movement
- Alternating pressure (active) air beds and mattresses (commonly used in healthcare settings to reduce and distribute pressure in hospitalised patients)
- Corrugated viscoelastic foam surfaces
- Special heel elevators and Prevalon boots
- Individual patient positioning plans and mattress selection in community settings such as residential aged care facilities.
What is the outcome of pressure ulcers?
- Prevention and early detection are crucial, as stage 3–4 ulcers take weeks to months to heal and can be resource-intensive and expensive to manage.
- Surgery is only indicated in patients whose wounds are refractory to non-invasive management; these patients also need to be fit for surgery.
- Infection and sepsis can be severe and life-threatening; systemic antibiotic therapy may be required.
- Vacuum pumps are not routinely used as they require input from experienced wound care nurses; improper use can lead to further exacerbation of pressure ulcers.