What is Chediak-Higashi syndrome?
Chediak-Higashi syndrome is a childhood disorder that interferes with immune system function. It is also known as Begnez-Cesar syndrome, leukocyte anomaly albinism or defect in natural killer lymphocytes.
It was first described in 1943 by Dr Beguez-Cesar.
Who gets Chediak-Higashi syndrome?
Chediak-Higashi syndrome is rare.
- An estimated 200–500 cases have been reported worldwide.
- The incidence is the same in males and females.
- It affects all races, but researchers suspect its occurrence may be under-reported.
What causes Chediak-Higashi syndrome?
Chediak-Higashi syndrome is an autosomal recessive condition caused by a mutation on the LYST gene. It is often due to parental consanguinity. The LYST gene affects the creation and maintenance of storage granules and causes problems with the transport of a protein across cells.
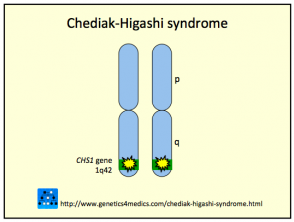
Genetics of Chediak-Higashi syndrome*
*Image courtesy Genetics 4 Medics
What are the clinical symptoms of Chediak-Higashi syndrome?
Signs and symptoms begin to affect children with Chediak-Higashi syndrome shortly after birth or by age five at the latest.
- Oculocutaneous albinism, or hypopigmentation of the hair, eyes and skin; hair is described as light in colour with a metallic sheen
- Prolonged bleeding and easy bruising due to platelet abnormalities
- Frequent viral, bacterial and fungal infections
- Photosensitivity
- Nystagmus: abnormal, involuntary eye movements
- Numbness/tingling in the limbs due to peripheral neuropathy
- Poor immunity due to abnormal function and shape of natural killer cells
Onset of Chediak-Higashi syndrome in adult life is associated with milder symptoms. These may include:
- Jaundice
- Skin infections
- Recurrent infections of the sinuses or respiratory tract
- Enlarged lymph glands
- Gum disease (gingivitis)
- Hyperhidrosis and miliaria
- Fever without infection.
Complications of Chediak-Higashi syndrome
The majority of patients (around 80%) will undergo an accelerated phase of Chediak-Higashi syndrome. This phase is marked by the nonmalignant reproduction of white blood cells in multiple body organs. This accelerated phase can be precipitated by the presence of a viral infection, and it is often fatal if it occurs in childhood. This phase is called haemophagocytic lymphohistiocytosis (HLH).
How is Chediak-Higashi syndrome diagnosed?
Diagnosis of Chediak-Higashi syndrome is made by:
- Examination of the white blood cells for the presence of large granules
- Light microscopy of the hair to find pigment clumping.
How is Chediak-Higashi syndrome treated?
Treatment for Chediak-Higashi syndrome may include:
- Cord blood or bone marrow transplant, which is considered the treatment of choice; it is more successful if done before a child reaches the accelerated phase of the disease
- Chemotherapy is needed to put hemophagocytosis (the HLH phase) into remission before a transplant can take place
- Avoidance of exposure to sunlight and sun protective measures
What is the outlook for Chediak-Higashi syndrome?
Without treatment, the outlook for Chediak-Higashi syndrome is poor. Around 50–85% of children with this disorder will enter the accelerated HLH phase. This process with fatal without treatment and most patients will die by the age of 10 years.