Background
Gout is a common disorder, which affects around 1% of the population. It is caused by excess uric acid, which exists as ionised urate in the blood. Saturated plasma urate (blood levels above 0.42 mmol/L) may slowly form monosodium urate (MSU) crystals that are deposited in the joints, kidneys, and soft tissues, eventually resulting in arthritis, kidney damage, and lumps under the skin respectively.
In healthy individuals, uric acid / urate is formed after eating certain high-protein foods. Usually most of the uric acid is then excreted by the kidneys in the urine. Excess urate in the blood can result from:
- A diet that is high in animal-based protein, especially meat and seafood.
- Moderate to high alcohol intake, especially of beer.
- High intake of fructose, a sugar found in sugar-sweetened soft drinks and fruit juices (apples and oranges).
- Being overweight – gout is associated with the metabolic syndrome.
- Some medications, including diuretics, low-dose aspirin and ciclosporin.
- Kidney disease can reduce urinary excretion of uric acid.
- Overproduction of uric acid can occur in disorders that cause high cell turnover, such as some myeloproliferative disorders (excessive numbers of cells produced by the bone marrow) and some types of anaemia (haemolytic anaemia and pernicious anaemia).
Other risk factors for gout include:
- Having a family history of gout.
- Age – in general, uric acid levels are elevated for 20 years before gout develops. In men uric acid levels rise at puberty so gout is often diagnosed in their 4th to 6th decade of life. Oestrogen protects young women from gout; uric acid levels rise at menopause and gout is often diagnosed in their 6th to 8th decade of life.
Clinical features of gout
In most cases, the first attack of gout presents with extreme pain and swelling in a single joint, often the big toe (podagra). The pain begins abruptly and the joint is red, hot, and extremely tender. Occasionally the first attack of gout affects multiple joints simultaneously. Patients may have a fever, particularly if many joints are involved. Untreated attacks of gout usually last 7-10 days, following which the patient may be symptom-free until the next attack.
Acute gout
Initially, attacks of gout may be months or years apart. An attack of gout can be brought on by:
- A sudden increase in blood urate level, e.g. after an episode of binge-drinking, eating a large quantity of high-protein food, dehydration, trauma, or starting a medication that raises uric acid.
- A sudden decrease in blood urate level, e.g. after starting a medication that lowers uric acid.
If gout remains untreated, the following complications can occur:
- Attacks become more frequent, last for longer, and involve more joints.
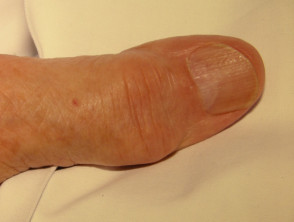
- Collections of MSU crystals, called tophi, develop in the soft tissues and appear as firm lumps under the skin. Tophi generally develop around 10 years after the first attack of gout in untreated patients and are commonly found around the elbows, hands, and feet. Tophi contain a white pasty material and as they enlarge they work their way towards the skin surface to drain. Small sinus tracts (tunnels) may develop and secrete white pasty material. Alternatively a large blister may form, which ruptures leaving a continuously draining ulcer.
- Tophi develop in and around the joints leading to joint destruction and chronic (long-term, continuous) joint pain and stiffness.
- Panniculitis (inflammation of the fat under the skin) is a rare complication of gout. This presents as nodular (lumpy) lesions of the legs that ulcerate and drain a fluid that contains MSU crystals.
- MSU crystals can be deposited in the kidneys producing inflammation and scarring (called chronic urate nephropathy). Kidney stones are also common in patients with gout.
Gouty tophi
More images of gouty tophi ...
How is the diagnosis of gout made?
- Gout is diagnosed in the initial attack by using a needle and syringe to extract a small sample of fluid from around the affected joint space. MSU crystals can be identified under the microscope. This test is also important to rule out other causes of an inflamed joint, such as infection.
- If a biopsy sample is taken, the specimen should be placed in alcohol, as formalin dissolves urate crystals.
- Joint x-rays may show findings consistent with gout, but these findings are not diagnostic on their own. Furthermore, early on in the disease, x-rays may be normal or show soft tissue swelling only.
- Urate levels may be elevated in the blood, but this finding alone is not diagnostic. In some cases, the level may even be below urate saturation.
What is the treatment for gout?
The treatment of gout is divided into 3 phases: treatment of the acute attack, uric acid-lowering therapy, and prevention of acute flares.
Treatment of an acute attack of gout
Options for treatment to relieve the pain of an acute attack of gout include:
- NSAIDs (non-steroidal anti-inflammatory drugs) – These are generally the medicines of choice for most patients who do not have underlying health problems. Aspirin should be avoided as it can alter urate levels and worsen the attack.
- Corticosteroids – If only one joint is involved, corticosteroids can be injected directly into the joint space. Otherwise, oral prednisone 20-40mg daily is prescribed for 10-14 days.
- Colchicine – Up until recently, colchicine was the treatment of choice for acute gout. However, due to recent safety concerns, colchicine is now only recommended if NSAIDs or corticosteroids are inappropriate. High dose colchicine therapy is no longer recommended because of its toxicity.
The above medicines do not prevent joint damage, tophi, or kidney disease.
Medicines to reduce uric acid
Long term management of gout focuses on lowering urate levels, aiming for levels under 0.36 mmol/L, or better still, under 0.30 mmol/L. These medicines can prevent attacks of gouty arthritis and prevent MSU crystals from being deposited in the tissues. Medicines that lower urate levels should not be started during an acute attack of gout; instead they should be started a few weeks after the attack has resolved.
Allopurinol
Allopurinol is an effective uric-acid lowering therapy, but it has a number of side effects and interactions with other medicines.
Dermatological side effects of allopurinol range from a mild morbilliform eruption (measles-like rash, which resolves when the drug is discontinued) to Stevens-Johnson syndrome / toxic epidermal necrolysis and drug hypersensitivity syndrome. Drug hypersensitivity syndrome is rare but potentially very severe. It usually occurs within the first 6 weeks of therapy but some cases have been reported up to 12 weeks after starting allopurinol.
The dose of allopurinol should start low at 100mg daily. The dose should be increased every 3-4 weeks, while monitoring blood urate level – aiming for a fall of under 0.04 mmol/L each month and eventual level below 0.36 mmol/L. Some patients may require doses of 600 to 900 mg daily to achieve this. The dose should be lower in those with kidney disease.
Febuxostat
Febuxostat (trade name Adenuric®) is a new medication for gout that may be used to reduce urate levels in patients with poor kidney function or intolerant of allopurinol. Phase III clinical trials have reported febuxostat to be more effective than allopurinol at a dose of 300mg. It is funded in New Zealand for treatment–resistant patients or those unsuitable for allopurinol, with Special Authority criteria.
Probenecid
Probenecid is an alternative uric acid lowering medicine with fewer significant side effects than allopurinol.
It is important to drink plenty of fluids while on probenecid, to flush out the uric acid and prevent crystals forming within the kidneys or urinary tract.
The starting dose of probenicid is usually 250 mg twice daily but it may need to be increased to up to 1 g twice daily.
Benzbromarone
Benzbromarone is a new medication for gout that may be used to reduce urate levels where allopurinol and/or probenecid are contraindicated, not tolerated, or are ineffective. Liver function must be monitored on benzbromarone, as it is reported to cause hepatic toxicity.
Prevention of acute flares
Acute flares of gout can be precipitated by the sudden reduction in blood urate that occurs when uric acid lowering medicines are started. For this reason it is important to take a low (preventative) dose of a NSAID or colchicine to reduce the likelihood of a flare developing. In patients unable to take either of these medicines, an oral corticosteroid can be considered. Patients who have only occasional attacks of gout, may only need to take these medicines for 2-3 weeks. Whereas patients with multiple tophi may need to continue treatment for months.
General measures in gout
Although lifestyle changes rarely result in adequate reduction in plasma urate without medication, the following are recommended.
- Weight loss in obese patients
- Reduction in alcohol intake
- Avoidance of soft drinks sweetened with fructose
- Restrict intake of liver, kidneys, fish, yeast extracts, red meat
- Consider alternative medication if on diuretic for hypertension