Hidradenoma papilliferum, also called papillary hidradenoma, is benign tumour arising from apocrine glands (see sweat gland lesions). The lesion is a small solitary dermal or subcutaneous nodule, most commonly on the vulva.
Histology of hidradenoma papilliferum
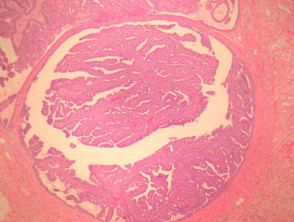
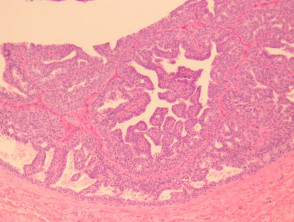
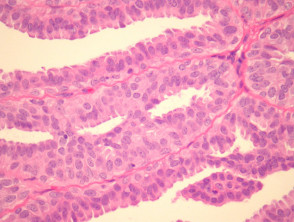
Hidradenoma papilliferum is a well-circumscribed dermal nodule, usually without connection to the overlying epidermis (figure 1). Tubules and broad, elongated fronds form an arborizing pattern and are lined with a double-layered epithelium (figures 2, 3). The inner layer is comprised of cuboidal myoepithelial cells and the outer is tall columnar apocrine cells with a pale eosinophilic cytoplasm, which may demonstrate decapitation secretion. Larger fronds may have a fibrous core. Fibrous tissue surrounding the tumour may be compressed to form a pseudocapsule.
Hidradenoma papilliferum pathology
Special studies of hidradenoma papilliferum
None are generally needed. Epithelial cells express keratin, EMA and CEA. GCDFP-15 (a marker of apocrine differentiation) is usually positive. Oestrogen, progesterone and androgen receptors may be positive. Myoepithelial cells express S-100 and smooth muscle actin. PAS positive granules are evident in the apices of apocrine cells.
Differential diagnosis of hidradenoma papilliferum
Syringocystadenoma papilliferum: Differentiating features of this crusted lesion include continuity of the lesion with surface epithelium and a prominent plasma cell infiltrate of the fibrous cores.
Malignant variant with intraductal carcinoma: Extensive infiltrative growth pattern with prominent mitotic activity and nuclear polymorphism.
Adenocarcinoma: Lacks a myoepithelial layer, shows marked nuclear atypia and an infiltrative growth pattern.