What is lymphoma?
Lymphomas are cancers that develop in the lymphatic system of the body. These cancers form when there is abnormal and excessive growth of B lymphocytes and T lymphocytes in the lymph nodes and other parts of the body. There are many different subtypes of lymphoma, categorised into Hodgkin lymphoma and non-Hodgkin lymphoma (NHL).
What is Hodgkin lymphoma?
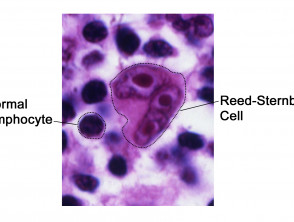
Hodgkin lymphoma is a B-cell lymphoma characterised by a tumour cell called the Reed-Sternberg cell [1]. These are large abnormal lymphocytes with multiple nuclei that are found on the histology of affected lymph nodes.
Reed-Sternberg cell
Hodgkin lymphoma typically presents with painless swelling of superficial lymph nodes or with an asymptomatic mass on a chest X-ray. Patients with Hodgkin lymphoma occasionally present with severe generalised pruritus or with skin lesions.
How is Hodgkin lymphoma classified?
There are two distinct types of Hodgkin lymphoma according to the World Health Organization (WHO) Classification of Tumours of Haematopoietic and Lymphoid Tissues [2]; these being:
- Classical Hodgkin lymphoma (95% of cases)
- Nodular lymphocyte-predominant Hodgkin lymphoma (5% of cases).
Classical Hodgkin lymphoma is further histologically classified into:
- Nodular sclerosis classical Hodgkin lymphoma
- Lymphocyte-rich classical Hodgkin lymphoma
- Mixed cellularity classical Hodgkin lymphoma
- Lymphocyte-depleted classical Hodgkin lymphoma.
Who gets Hodgkin lymphoma?
Hodgkin lymphoma is a relatively rare disease, accounting for approximately 0.6% of all cancers diagnosed in the developed world annually.
- Around 66,000 new cases of Hodgkin lymphoma were diagnosed worldwide in 2012.
- Around 75 New Zealanders are diagnosed with this disease each year [1].
- The incidence rates of Hodgkin lymphoma are highest in Northern America and lowest in Eastern Asia [3]. This variation between countries may be due to different prevalence of risk factors, use of screening, and/or diagnostic methods.
Hodgkin lymphoma develops in two main age groups.
- Hodgkin lymphoma is mostly diagnosed in young adults aged 15–35 years but can also develop in people over 55 years of age.
- The younger age group tends to be more commonly affected by the nodular sclerosis subtype [4].
- Hodgkin lymphoma is generally more common in males, although the nodular sclerosis subtype is seen more frequently in females.
What causes Hodgkin lymphoma?
Hodgkin lymphoma is caused by a change in the DNA of a B-cell lymphocyte. This mutation causes a large number of abnormal and oversized B cells to accumulate in the lymphatic system, and, over time, spread to other organs. It is not clear what causes DNA mutation.
- A family history of a specific subtype of Hodgkin lymphoma is most strongly associated with the risk for that subtype, supporting the likelihood of a genetic predisposition [5,6].
- The risk of lymphoma increases slightly in patients with chronic infections or autoimmune diseases.
- Those with immune suppression, such as people who have received long courses of chemotherapy for other diseases, or who are infected by viruses such as human immunodeficiency virus (HIV) or Epstein-Barr virus (EBV), are also at increased risk of developing lymphoma [7]. See also, Epstein–Barr virus-associated lymphoproliferative disorders.
What are the clinical features of Hodgkin lymphoma?
Hodgkin lymphoma usually starts within a single lymph node and then progresses to nearby lymph nodes via the lymphatic channels before spreading to distant sites and organs [8,9]. It typically presents with painless swelling of superficial lymph nodes (in the neck, axilla, or groin) or as an asymptomatic mass seen on a chest X-ray.
Some patients present to their doctors with non-specific, or 'B', symptoms. They can have one or more of the following symptoms:
- Fevers
- Drenching night sweats
- Unintentional weight loss
- Lethargy.
Occasionally, patients can present with symptoms and signs that reflect the involvement of organs in the disease such as:
- Jaundice and itching due to liver involvement
- Tetany (muscular spasms) due to high levels of calcium
- Tiredness due to anaemia
- Oedema due to kidney involvement.
Cutaneous manifestations of Hodgkin lymphoma
Direct cutaneous infiltration
- Cutaneous Hodgkin lymphoma is very rare.
- The chest is the most common site.
- It usually presents as dermal papules and plaques.
- There may be a single nodule or a cluster of subcutaneous nodules.
- Lesions may ulcerate.
Nonspecific cutaneous signs
Nonspecific cutaneous signs include:
- Generalised pruritus or excoriations
- Acquired ichthyosis (very dry skin)
- Hyperpigmentation
- Spontaneous urticaria.
Eczematised lesions
-
- Eczematised lesions may be paraneoplastic.
- They are usually noted just prior to or at the time of the diagnosis of advanced Hodgkin lymphoma associated with systemic nodal disease.
- Itchy papules or scaly or lichenified plaques tend to be located along the drainage area of the affected lymph nodes.
- Lesions may be impetiginised due to staphylococcal infection.
- They may be solitary, grouped, or (rarely) generalised [10–12].
Cutaneous lesions in Hodgkin lymphoma
How is Hodgkin lymphoma diagnosed?
A thorough history and physical examination is the initial step in the diagnosis of Hodgkin lymphoma, which is confirmed by the presence of Reed-Sternberg cells on the pathological examination of a lymph node biopsy [8].
- A full blood count and inflammatory markers are used to check for signs of anaemia and inflammation.
- The lymph node evaluation can be an excisional biopsy (where an entire lymph node is removed), an incisional biopsy, ie where part of a lymph node is removed), or a core biopsy (where part of a lymph node is removed using a wide needle).
- A skin biopsy of an infiltrated nodule may be diagnostic of Hodgkin disease in patients with direct cutaneous infiltration with Hodgkin lymphoma. Typically, histology reveals Reed-Sternberg cells within an infiltration of small lymphocytes, histiocytes, eosinophils, and plasma cells.
What is the differential diagnosis for Hodgkin lymphoma?
Any disease presenting with enlarged lymph nodes with constitutional symptoms, such as fevers and weight loss, should be considered in the differential diagnosis of Hodgkin lymphoma [12].
Non-Hodgkin lymphoma
- NHL is difficult to clinically differentiate from Hodgkin lymphoma, and the diagnosis requires pathological confirmation.
- Hodgkin lymphoma tends to spread from one lymph node chain to another, whereas extra-nodal sites are usually involved in NHL.
- Patients with Hodgkin lymphoma tend to be younger than patients with NHL.
Other malignancies
- Many malignancies may present with enlarged lymph nodes due to metastasis.
- Head and neck cancers can often spread to the cervical lymph nodes.
- Breast cancer commonly spreads to the axillary lymph nodes.
- The best way to differentiate Hodgkin lymphoma from other malignancies is to do a lymph node biopsy.
Infectious mononucleosis
- The enlarged lymph nodes in infectious mononucleosis are usually tender.
- Patients with infectious mononucleosis typically present with a sore throat.
- The infection is diagnosed by blood count findings and positive serology for EBV.
Reactive lymph nodes
- Lymph nodes can also become enlarged from any infectious or inflammatory causes.
- These enlarged lymph nodes typically return to normal within a few weeks.
- When enlarged lymph nodes or symptoms persist, a lymph node biopsy can be considered to rule out Hodgkin lymphoma.
What is the treatment for Hodgkin lymphoma?
The treatment for Hodgkin lymphoma may include [12]:
- Chemotherapy
- Radiation therapy
- Surgery
- A combination of these options.
Chemotherapy involves either taking oral tablets or the drug is injected into a vein or muscle, depending on the type and stage of the cancer being treated.
Radiation therapy can be used to treat solitary or localised specific skin lesions. For a pregnant woman with Hodgkin lymphoma, radiation therapy should be postponed until after delivery, if possible, to avoid any risk to the fetus.
- Other treatment options, especially for pregnant patients, include watchful waiting (monitoring) and systemic steroids.
- Treatments for Hodgkin lymphoma currently being evaluated include radiation therapy with stem cell transplant and monoclonal antibody therapy.
Non-specific cutaneous symptoms may be treated with:
- Topical corticosteroids
- Emollients
- Antipruritic creams
- Oral antihistamines for pruritus
- Antibiotics for secondary bacterial infection.
What is the outcome for Hodgkin lymphoma?
Hodgkin lymphoma can usually be cured if found and treated early. The prognosis of Hodgkin lymphoma has improved in recent decades, with a current 5-year survival rate of over 80%.
The prognosis depends largely on the following:
- The patient’s signs and symptoms
- Their age, sex, and general health.
- The type of Hodgkin lymphoma
- The stage of cancer.
Cutaneous Hodgkin lymphoma usually represents advanced disease and carries a poor prognosis despite aggressive treatment [1].