What are non-albicans candida infections?
Non-albicans candida infections are fungal infections caused by the Candida species of yeast other than C. albicans. These include:
- C. glabrata
- C. krusei
- C. kefyr
- C. parapsilosis
- C. tropicalis
- C. dubliniensis
- C. guilliermondii
- C. orthopsilosis[1].
The incidence of non-albicans candidiasis has been increasing over recent years.
Who gets non-albicans candida infections?
Of the known non-albicans candida species, only C. tropicalis, C. parapsilosis, and C. orthopsilosis can be found on healthy skin (commensal microorganisms) and can become pathogenic [2].
Infections typically develop in the context of wounds or broken skin, pre-existing illness, or immunosuppression.
- Virulence factors such as biofilm formation, hydrolytic enzymes, and adherence to host tissue contribute to the transition from commensal to pathogenic species [3].
- Factors that have led to an increase in non-albicans candida infections include widespread use of broad-spectrum antibiotics, empirical use of antifungal drugs, and indwelling catheters and other medical devices [1,3].
What are the clinical features of non-albicans candida infections?
The clinical features and complications of non-albicans candidiasis are usually very similar or indistinguishable from candidiasis caused by C. albicans [3].
Vulvovaginal candidiasis
Vulvovaginal candidiasis is one of the most frequent infections experienced by adult women [4]. It presents with vulval irritation, itching, soreness, discomfort with sexual activity (dyspareunia), and a curdy-white vaginal discharge [4]. Many non-albicans species have been identified in vulvovaginal candidiasis, with most cases associated with C. glabrata, C. krusei, C. tropicalis, C. parapsilosis, and C. dubliniensis.
- C. glabrata accounts for 50–67% of reported non-albicans vulvovaginal candidiasis [4].
- Non-albicans candida species are more often isolated from asymptomatic women than from women with vulvovaginitis [4,5].
- Some studies relating non-albicans species to symptomatic vulvovaginitis have shown that non-albicans infections can present with milder symptoms compared with C. albicans [5].
- Treatment failure is a common feature [4].
Oral candidiasis
Candida species are a part of the normal oral flora of healthy individuals. Oral candidiasis is caused by an overgrowth of Candida species in the mouth. The two main forms are white oral candidiasis (pseudomembranous candidiasis, hyperplastic candidiasis) and erythematous oral candidiasis (atrophic candidiasis, median rhomboid glossitis, angular cheilitis, linear gingival erythema). Other forms are chronic mucocutaneous candidiasis, cheilocandidiasis (candida affecting lips), and chronic multifocal candidiasis [6].
Non-albicans species implicated in oral candidiasis include:
- C. dubliniensis
- C. glabrata
- C. kefyr
- C. parapsilosis
- C. stellatoidea
- C. tropicalis [6].
Systemic candidiasis
Systemic candidiasis is the invasion and growth of Candida in specific organ systems (also called disseminated candida) or the bloodstream (candidaemia). It is an opportunistic infection.
- Increasing prevalence of C. krusei, C. glabrata, C. tropicalis, and C. parapsilosis causing systemic candidiasis is reported worldwide [7-9].
- Malignancy is one of the major underlying causes; systemic candidiasis is associated with a 30–50% mortality rate in cancer patients [8].
- Other risk factors include exposure to quinolones or b-lactamase inhibitors and the presence of central venous catheters [9].
How are non-albicans candida infections diagnosed?
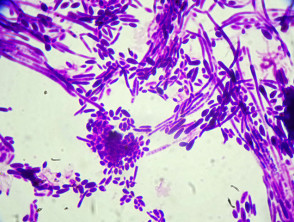
All candida infections are diagnosed by their typical clinical features and by seeing pseudohyphae and yeast forms on microscopy of swabs and scrapings. See laboratory test for fungal infections.
- Fungal cultures identify Candida, rule out bacterial infection, and determine topical or oral antifungal sensitivities [10].
- Non-albicans species identification can be determined using biochemical and molecular biology techniques including polymerase chain reaction (PCR) [1,3].
Non-albicans candida in the laboratory
What is the treatment for non-albicans Candida infections?
Candida infections are treated using the three approved classes of antifungals: azoles, echinocandins, and amphotericin B. Resistance to azoles, while rare in C. albicans, is frequent with non-albicans species [1,3].
The most common topical antifungal medications used in treatment trials for cutaneous candidiasis are clotrimazole, nystatin, and miconazole, and they show equivalent efficacy [11].
Boric acid intravaginal suppositories have been reported to achieve mycological cure for vulvovaginal candidiasis caused by C. glabrata, C. tropicalis, and C. lusitania. [12].
Systemic/oral antifungal medications for cutaneous candidiasis include fluconazole and itraconazole. Voriconazole and posaconazole are reserved for serious systemic candidiasis.
Candida auris: an emerging species
C. auris is a multidrug-resistant pathogen increasing in incidence since its initial isolation and recognition from an ear swab in 2009 [13]. Systemic candidiasis in critically ill patients on broad-spectrum antibiotics and/or antifungals has been the most common presentation. Skin and soft tissue infections including wound infections, have also been recognised [13].
- C. auris can colonise body sites including nose, groin, axilla, and rectum [13].
- Risk factors for C. auris infection include contact with infected persons, serious underlying medical conditions, invasive procedures including surgery and indwelling catheters, immunodeficiency, and immune suppression [13].
- Infection control and prevention is important to control outbreaks in healthcare facilities [14].
Treatments for C. auris are extremely limited; echinocandins are the most frequently recommended option, though several strains are believed to be resistant to all antifungals. Off-patent or repurposed drugs are being investigated for the treatment of C. auris infections [15,16].