Introduction
Patients who have received an organ transplant have a higher risk than normal for developing skin cancers, in some cases up to 65 times the risk, compared with non-transplant patients. In particular, transplant recipients have a significantly increased risk of developing squamous cell carcinomas. SCC is more likely to spread (metastatic SCC) in organ transplant recipients and may lead to the death of the patient.
Organ transplant recipients are also at increased risk for other types of skin cancers, particularly melanoma. These may occur on any site on the body. All histological subtypes are seen. Melanoma can be very difficult to diagnose in organ transplant recipients, leading to a low threshold to excise any unusual or changing lesion. Melanoma tends to be thicker and more advanced on diagnosis than in non-transplant patients, and these tumours may behave aggressively in organ transplant recipients.
Preventative measures, early detection, regular skin checks and appropriate early treatment of skin cancers are essential to minimise the harm caused by these cancers. Other tumours occurring in organ transplant recipients include Merkel cell carcinoma and Kaposi sarcoma.
Why are transplant patients at higher risk of skin cancer?
Transplant patients require the long-term use of immunosuppressant medications to prevent organ rejection, but they impair the capacity of the immune system to repair or destroy UV-damaged cells, allowing these damaged cells to develop into cancers. Ultraviolet (UV) exposure is the major factor in the development of skin cancers in both transplant and non-transplant patients.
It is also possible that the immunosuppressant medications directly cause cancer generating changes in cells. Additionally, human papillomavirus (HPV), which causes warts, may also be involved in the development of skin cancers in transplant recipients.
Who is at the highest risk of skin cancer?
Patients who have been receiving immunosuppressant medications for longer periods tend to have the highest incidence of skin cancers. More than 75% of renal transplant patients survive ten years or longer and are at significant risk. Other risk factors for skin cancer include:
- Older age (possibly due to greater cumulative sun exposure)
- History of skin cancers or pre-cancerous lesions before the transplant
- Fair skin (Fitzpatrick skin type I-III); it has been estimated that about half of white-skinned organ transplant recipients develop skin cancer
- History of significant UV exposure from sun or sunbeds
- Infection with the HPV (wart) virus
- Low CD4 cell counts
- Heart and lung transplant recipients (who tend to have higher levels of immunosuppressant medication).
It has been noted that well-matched heart and lung recipients have a slightly higher risk than less well-matched recipients.
Preventing skin cancer in transplant patients
Being sun-smart is vital for transplant patients. The incidence of skin cancers may be greatly reduced by following preventative measures whenever out of doors, including:
Always wear sunscreen
- Sunscreen should be rated SPF30+ and should be broad spectrum (blocking both UVA and UVB radiation). You should apply sunscreen 15-30 minutes before going outside and then again immediately before going outside. Sunscreen needs to be reapplied regularly during the day (2-hourly in sunny weather, otherwise 3 to 4-hourly). Daily application to the face and hands regardless of your intended activities should be considered.
Avoid sun exposure
- This is especially important during the middle of the day, between 11 am and 4 pm, when UV radiation levels are at their highest. If you are outdoors during these times, stay in the shade. Check the weather reports to find out ultraviolet index or sun protection alerts – take these seriously.
Cover up well
- Wear with long-sleeved shirts and pants. Dark coloured, tightly woven material provides the most UV protection. If possible try to wear sun protective clothing that has an Ultraviolet Protection Factor (UPF) rating of 40-50+.
Always wear a hat when outdoors
- Choose a hat with tightly woven material that shades your face, nose, neck and ears.
Wear sunglasses
- Sunglasses provide the best protection to the delicate skin around the eyes. Choose glasses that are close fitting with large lenses. Wrap around style glasses provides the best protection.
Detecting skin cancers
Early detection and treatment of cancerous and pre-cancerous skin lesions are essential to minimise the harm caused by skin cancers. Transplant patients should perform a skin self-examination every month, concentrating particularly on areas that are normally most exposed to sunlight, such as the backs of the hands, forearms, head and neck, upper chest and back and, in women, the lower legs. They should promptly report any new lesions to their dermatologist, family doctor, or specialist.
Recognising skin cancers
Examples of some of the common skin cancers in transplant recipients are illustrated below.
Squamous cell carcinoma
- Raised, crusting non-healing sore or lump
- Vary in size from few millimetres to several centimetres in diameter
- Can grow rapidly within a few weeks
See more information about cutaneous squamous cell carcinoma.
Squamous cell carcinoma (SCC)
Basal cell carcinoma
- Pale red or pearly smooth lump; often on the head or neck
- Pink, scaly patches; more often on trunk and limbs
- Usually slow growing
See more information about basal cell carcinoma.
Basal cell carcinoma (BCC)
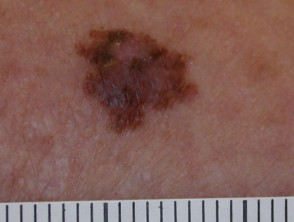
Melanoma
- A new mole or freckle, or an existing mole that is changing in shape or size
- Often has irregular edges with multiple colours (red, tan, black, brown, grey, white) within the spot
See more information about melanoma.
Melanoma
Actinic keratoses
- Rough, scaly spots
- Usually flat
- Not cancerous but can develop into squamous cell carcinomas
See more information about actinic keratoses.
Actinic keratoses in transplant patients
Treating skin cancers in transplant patients
Skin cancers are often very aggressive in transplant patients and are associated with a high risk of metastases (spreading) and recurrence. It is important that any skin cancer is treated at an early stage to minimise this risk.
Most skin cancers in transplant patients are treated by surgical excision or Mohs micrographic surgery. Surgery allows the specimen to be examined by the pathologist to ensure that the cancer has been completely removed. In some cases, further surgery or radiotherapy may be required. Occasionally, some lower-risk skin cancers, such as. Small tumours on the trunk may be treated with electrodesiccation and curettage.
Actinic keratoses and warty lesions should also be treated aggressively to try to minimise the risk of these areas developing into squamous cell carcinomas. Treatments for these may include:
- Cryosurgery
- Electrodesiccation and curettage of thicker lesions
- Topical 5-fluorouracil (Efudix™) twice daily for 4 to 6 weeks, repeated as necessary
- Topical imiquimod (Aldara™) is applied to small areas with variable response
- Photodynamic therapy may be appropriate for flat lesions, e.g. SCC in situ.
Transplant recipients who have high-risk squamous cell carcinomas or who develop many squamous cell carcinomas within a year (usually more than five lesions per annum), may be commenced on an oral retinoid such as acitretin or isotretinoin. These medications have been shown to reduce the number of new skin cancers that develop, however they are only effective while they are being taken. When the retinoid treatment is stopped, the rate at which skin cancers develop returns to pre-treatment levels. The dose of the retinoid may need to be adjusted if adverse effects are troublesome.
Reducing the levels of immunosuppressive medications, or replacing them with drugs with a lower risk of skin cancer, may be considered for some patients with potentially life-threatening skin cancers. This might improve the outcome from the skin cancer, by allowing the immune system to fight the cancer cells. As there are risks associated with reducing immunosuppression, this is only carried out in close collaboration with the transplant physician and after careful discussion of the potential risks and benefits with the patient.
There is increasing support for the use of mTOR inhibitors such as sirolimus for immunosuppression in solid organ transplant recipients that are developing multiple skin cancers. These drugs have some anticancer properties, and reduced numbers of skin cancers have been reported in organ transplant recipients receiving them. However, mTOR inhibitors have significant adverse effects such as peripheral oedema and papulopustular acne-like reactions, and they are not always suitable.