What is a spondyloarthropathy?
Spondyloarthropathy refers to a group of five seronegative inflammatory rheumatic disorders that are related in disease manifestation and genetic susceptibility [1]. The spondyloarthropathies include:
- Ankylosing spondylitis
- Psoriatic arthritis
- Reactive arthritis
- Enteropathic arthritis (arthritis associated with inflammatory bowel disease)
- Undifferentiated spondyloarthropathy.
Spondyloarthropathy is also called spondyloarthritis.
Who gets spondyloarthropathy?
Ankylosing spondylitis affects 0.1–1.4% of Caucasians. It is three times more common in males than in females. Ankylosing spondylitis commonly occurs in several members in a family. About 95% of individuals affected by ankylosing spondylitis carry the tissue antigen human leukocyte antigen B27 (HLA-B27), which is associated with inflammatory conditions.
Spondyloarthropathies that are less frequently associated with HLA-B27 are psoriatic arthritis and reactive arthritis, the prevalence of which is around 2% in the general population [2].
What causes spondyloarthropathy?
The exact aetiology and pathogenesis of the spondyloarthropathies is undetermined. There is clear evidence that genetic background and environmental factors trigger proinflammatory cytokines, and these lead to an increased susceptibility to spondyloarthropathies [2]. There is a close link between ankylosing spondylitis, psoriasis, and Crohn disease. This link suggests that the pathogenesis of ankylosing spondylitis involves an immune reaction within the gut or the skin that may be influenced by microbial responses [3].
What are the clinical features of spondyloarthropathy?
Spondyloarthropathy syndromes are characterised by axial arthritis (which affects the lower back) or peripheral arthritis (which affects the wrists, ankles, knees, and elbows).
Patients generally complain of inflammatory back pain in the spine or sacroiliac joints (which connect the spine, hips, and sacrum).
The onset of back pain is usually before the age of 45 years [2].
Peripheral arthritis can affect small and large joints in an asymmetrical pattern.
Patients may also present with:
- Enthesitis (tenderness at where the tendons and ligaments attach to the bone) and heel pain
- Tenosynovitis (inflammation and swelling around a tendon)
- Dactylitis (swelling of the entire digit; ie, the ‘sausage digit’)
- Extra-articular manifestations (symptoms not related to the joints; eg, skin rash, inflammatory bowel disease, and uveitis)
- An immunogenetic association with the HLA-B27 antigen [4,5].
What are the skin conditions associated with spondyloarthropathy?
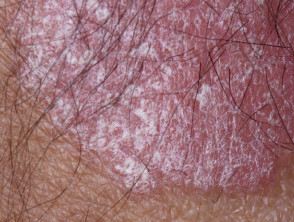
Psoriatic arthritis is strongly associated with chronic plaque psoriasis. Psoriatic arthritis more commonly develops after psoriasis, but arthritis can precede or accompany the skin disease. Patients with psoriatic arthritis usually have a family history of psoriasis and are more likely to have nail psoriasis than psoriatic patients without psoriatic arthritis [6].
Skin changes include:
- Erythematous plaques with a silvery-white scale
- Nail disease (oil spots, pitting, and crumbling)
- Sterile pustules.
Psoriasis in a patient with ankylosing spondylitis
Enteropathic arthritis can present with:
Mucocutaneous manifestations for reactive arthritis (associated with chlamydia infection) include:
- Oral ulcers
- Keratoderma blennorrhagicum (a painless papulosquamous eruption on the palms or soles)
- Circinate balanitis (vesicles or shallow ulcerations on the glans penis)
- Nail manifestations with pitting and onycholysis or subungual keratosis [1,5].
What are the complications of spondyloarthropathy?
Complications of axial spondyloarthritis include reduced bone mineral density, fractures, neurological manifestations, and renal disease. Low bone mineral density is commonly seen within the first 10 years of the disease. Spinal fractures can result in spinal cord injuries or spinal nerve compression.
Rarely, glomerulopathy, immunoglobulin A nephropathy, and renal amyloidosis occur in ankylosing spondylitis [7].
How is spondyloarthropathy diagnosed?
Spondyloarthropathies are diagnosed according to the Assessment of Spondyloarthritis International Society (ASAS) classification criteria [8]. These criteria only apply to patients aged under 40 years old or those with inflammatory back pain for over 3 months. The criteria include imaging, HLA-B27 status, and the features of spondyloarthropathy.
Imaging typically includes plain radiographs and magnetic resonance imaging. Sacroiliitis (inflammation of the lower spine) on plain radiography is specific for spondyloarthropathies. It may take several years before sacroiliitis is visible on imaging.
Laboratory evaluations should include a full blood count, a complete metabolic panel, and erythrocyte sedimentation rate (ESR) or C-reactive protein (CRP). The ESR and CRP are elevated in about 50% of patients with spondyloarthropathy. Elevated CRP is a good predictor of radiographic progression and better response to tumour necrosis factor (TNF) inhibitors [2].
What is the differential diagnosis for spondyloarthropathy?
The differential diagnoses for spondyloarthropathies is based on the distribution of the affected joints.
Axial disease
Differential diagnoses to consider include:
- Mechanical back pain — this is usually brief and with a history of a specific injury
- Fibromyalgia and myalgia — there is a lack of imaging changes and a minimal response to anti-inflammatory treatment
- Vertebral compression fracture — this occurs in patients with low bone mass due to osteoporosis or previous trauma.
- Osteitis condensans ilii — this is a radiological finding that occurs in women who have had more than one child and shows sclerosis on the iliac part of the sacroiliac joint
- Familial Mediterranean fever — these patients can develop back pain, peripheral arthritis, and sacroiliitis on imaging; they can be distinguished clinically through their family history of familial Mediterranean fever [2].
Peripheral joint disease
Differential diagnoses to consider include:
- Rheumatoid arthritis — this is symmetrical and polyarticular arthritis with radiographic changes, that is positive for rheumatoid factor and anti-citrullinated peptide antibodies
- Osteoarthritis — where symptoms worsen with activity
- Behçet syndrome — an asymmetrical, non-erosive arthritis that is most often seen in the descendants of those who lived along the ancient silk road from eastern Asia to the Mediterranean
- Crystalline arthropathy (gout) — this is typically monoarticular and intensely inflammatory arthritis that affects the feet
- Sarcoidosis — an acute polyarthritis that usually involves the soft tissue around the joints (periarthritis) in conjunction with erythema nodosum and acute uveitis [7].
What is the treatment for spondyloarthropathy?
The goal of treatment for spondyloarthropathies is to improve function, decrease pain, and reduce the risk of complications. Management should include lifestyle interventions, including an exercise program to maintain posture, strength, and range of movement. Patients should also be monitored for osteoporosis and encouraged to cease smoking.
Non-steroidal anti-inflammatory drugs (NSAIDs) are considered to be the first-line treatment for axial ankylosing spondylitis. They are quite effective, reducing pain, tenderness, and stiffness in 80% of patients. Patients who do not respond to NSAIDs may benefit from anti-TNF-alpha therapy, such as infliximab, etanercept, or adalimumab. These can reduce the spinal and peripheral joint inflammation of ankylosing spondylitis and control extra-articular symptoms.
Disease-modifying anti-rheumatic drugs (DMARDs) include sulfasalazine and methotrexate. Intra-articular corticosteroid injections have a modest benefit for peripheral arthritis [9].
The treatment for psoriatic arthritis targets the joints and skin lesions. Anti-TNF-alpha therapy for psoriatic arthritis has been a significant advance, resulting in a significant improvement in symptoms and a delay in progression of the disease. Secukinumab, an anti-interleukin-17A monoclonal antibody, is effective at treating psoriasis and psoriatic arthritis.
The management of reactive arthritis involves assessing and treating an active infection. Chlamydia infections should be treated with antibiotics. There is no evidence to support the use of antibiotics for treatment of urogenital or enteric forms of reactive arthritis. High-dose NSAIDs are also used to treat patients with reactive arthritis. Indomethacin 50–75 mg twice daily is commonly used. Persistent reactive arthritis may respond to DMARDs, such as sulfasalazine, azathioprine, or methotrexate [9].
Enteropathic arthritis is also treated with NSAIDs and cyclooxygenase-2 inhibitors, but these can cause flare-ups of inflammatory bowel disease. DMARDs are beneficial for gastrointestinal and joint involvement. Anti-TNF agents can be used if traditional DMARDs fail; however, there have been rare cases of inflammatory bowel diseases precipitated by etanercept. Total colectomy (removal of the affected colon) does not improve axial involvement in inflammatory bowel disease [5].
What is the outcome for spondyloarthropathy?
The progression of ankylosing spondylitis is highly variable. It may result in the fusion of sacroiliac joints and the vertebral column, also known as a ‘bamboo spine’. Patients who have frequent episodes of iritis, hip involvement at presentation, peripheral joint involvement, and high inflammatory markers at baseline tend to have a poorer prognosis [10].
At least 20% of patients with psoriatic arthritis will develop severe and disabling disease. Up to 7% of these patients may require joint surgery, with the most common being hip arthroplasty [11].
Approximately 50% of patients with reactive arthritis can expect symptoms to resolve in the first 6 months; however, 30–50% will develop chronic arthritis [12].
The prognosis of enteropathic arthritis is determined by the severity of the underlying bowel disease. Patients with well-controlled inflammatory bowel disease rarely develop severe enteropathic arthritis [5].