What is tuberculosis?
Tuberculosis (TB) is a serious bacterial infection with Mycobacterium tuberculosis (M. tuberculosis). Active systemic infection can cause serious illness and death if unrecognised and untreated. It can also spread to other people. Symptoms of an active systemic infection can include:
- Fever, night sweats
- Cough
- Chest pain
- Cough up sputum and/or blood
- Weakness, fatigue
- Weight loss, loss of appetite.
Tuberculosis typically affects the lungs but can involve any part of the body including the skin (Cutaneous tuberculosis).
What is tuberculosis screening?
Tuberculosis screening is the examination and investigation of a patient who does not have symptoms of active TB. Screening is undertaken to identify and treat latent TB so that it can be effectively treated before it becomes an active infection.
What is latent tuberculosis?
Latent tuberculosis occurs when patients carry live M. tuberculosis bacilli without knowing they are infected because their immune system has contained but not killed the bacteria. In healthy people, tubercle bacilli can remain alive in the body without causing disease for many years. Latent TB is not contagious.
If the balance between the immune system and the tubercle bacilli is disturbed, for example, by immunosuppressive drugs or other immune-altering treatments (eg, biologics), latent TB may become active.
Who is at risk from tuberculosis?
Active or latent TB infection is not common in New Zealand and other developed countries but continues to be reported in certain population groups. Risk factors for acquiring tuberculosis include:
- Close contact with a patient with active TB
- Living in or visiting a country or community where TB is common
- Living in a crowded community, including an institution such as a rest home, long-stay hospital, prison
- Working in hospitals and healthcare environments
When should tuberculosis screening be undertaken?
Tuberculosis screening should be undertaken in people at risk of tuberculosis and in people at risk for converting undetected latent TB to active TB. Examples include:
- Treatment with corticosteroids, biologics especially Tumour Necrosis Factor-alpha (TNFα) inhibitors, and immune-suppressing agents such as azathioprine, ciclosporin, mycophenolate or chemotherapy
- Illness, particularly human immunodeficiency virus (HIV) infection, leukaemia, lymphoma, diabetes, alcoholism, and renal failure
- Debility (old age, very young age, and longterm or heavy smokers).
What tuberculosis screening tests are performed?
After taking a history and general examination, the main TB screening tests are:
- Chest X-ray
- Tuberculin skin test (Mantoux test)
- TB blood test (in adults) - interferon-gamma release assay.
Skin testing and TB blood tests are usually positive in patients with latent TB; they demonstrate prior infection and a good level of immunity to it. The tests are also positive in patients with active TB.
The test results may require expert interpretation. Other tests may also be required, depending on symptoms.
Chest X-ray
Latent TB can be suspected on chest X-ray if any of the following features is/are present:
- Fibrotic area
- Apical scarring
- Blunted costophrenic angle
- Calcification
- Pleural thickening.
Patients with active TB may have cavitations or other signs on X-ray. A patient with latent TB may have a normal chest X-ray.
Tuberculin skin testing
The tuberculin skin test or Mantoux test contains a purified protein derivative (PPD) of TB bacteria, so it is also called a PPD test. The test material does not contain live bacteria and cannot cause TB. The test is undertaken by specially trained laboratory technicians and other healthcare workers.
- The test is usually performed on the inner aspect of a forearm.
- The selected area is first cleaned using an alcohol swab.
- 0.1 ml tuberculin (PPD) is injected intradermally, raising a bleb 6–10 mm in diameter.
The test site is inspected 2-3 days later. The diameter of hard skin thickening is recorded in millimetres. The test is classified as negative (no induration or less than 5 mm induration ) or abnormal (more than 5 mm induration). Abnormal tests may take weeks to subside and can leave a mark or scar. A Mantoux test will be positive after effective BCG immunisation.
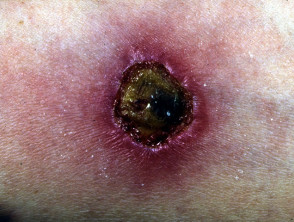
Severe Mantoux test reactions (active TB)
TB blood test
The usual TB blood test is interferon-gamma release assay (IGRA). There are several options, including QuantiFERON Gold™. One advantage of IGRA over skin testing is that it is not positive after BCG immunisation. A disadvantage is the difficulty and expense of conducting the test accurately.
Test results may be positive (infection is likely), negative (it is unlikely), indeterminate or borderline (uncertain). Borderline reactions are more often observed in patients taking immunosuppressive drugs, systemic steroids and antimalarial medications in patients that do not have tuberculosis. The test should be repeated at a later date, as a precaution.
My tests are negative. Can I be sure I don't have tuberculosis?
Even if initially negative, TB tests should be repeated from time to time in patients who are at risk of being infected with TB and in those who are at risk of latent TB converting to active TB.
What happens if tests are positive?
If any of the screening tests are positive, the result should be evaluated by a physician. Further tests and follow-up may be appropriate.
Treatment of TB is recommended for patients with active TB and in those at risk for the conversion of latent TB to active TB, for example, if they have a chronic immunodeficiency illness or treatment with an immunosuppressive drug.
The usual treatment is either isoniazid for 6 months, rifampicin for 3 months, or a combination. Guidelines vary for different populations, and if the patient is pregnant or has liver disease (see references).
Should the tuberculosis screening tests be repeated?
Tuberculosis testing should be repeated every year or so in patients on immune suppressive medications or in other patients at significant risk of active TB.