What is whole slide imaging?
Whole slide imaging is the software manipulation of digital images of tissue sections that have been scanned at various magnifications. This enables the viewer to zoom in on areas of interest, thereby simulating the examination of glass slides under a traditional microscope. Magnifications of up to × 60 can be achieved. A few modern scanners can also do x 100 for blood smears and bone marrow aspirations.
Whole slide imaging is also called virtual microscopy.
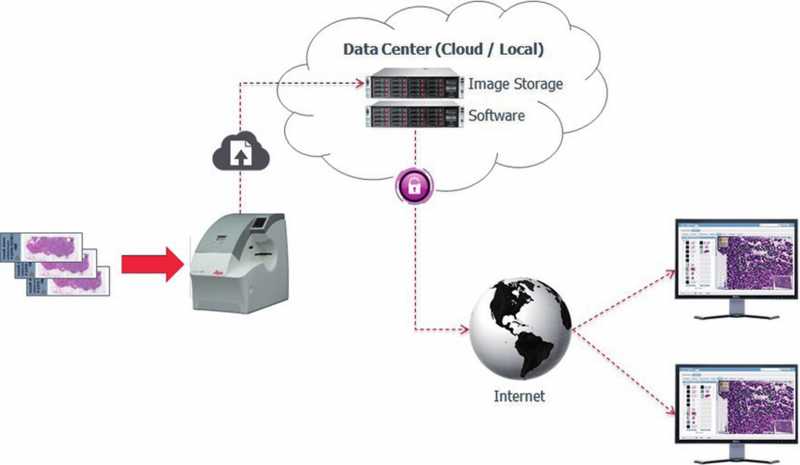
Courtesy of Colin Doolan, Leica Biosystems
Why use whole slide imaging?
Advantages of using whole slide digital images for microscopic examination of pathology specimens include:
- They are easily duplicated
- They do not deteriorate or break
- They can be stored, catalogued and managed with relative ease
- They are easily accessible via the internet, in spite of distant geographic locations.
The US Food and Drug Administration (FDA) permitted the marketing of whole slide imaging systems for use in pathological diagnosis in April 2017.
Dermatopathology is ideally suited to whole slide imaging for diagnoses, due to high case volume, low slide count and small specimen size in this speciality.
How can whole slide imaging be used?
Teaching, testing and e-learning
Computers are now readily available in educational institutions and are less costly than microscopes.
- Whole slide imaging makes it possible to provide an unlimited number of students and residents access to slides from rare cases that they would not traditionally view, and without the risk of valuable glass slides fading or breaking.
- All of the participants can view the same slide, ensuring that they benefit from exposure to the correct information.
- Software permitting 360-degree rotation of images allows them to be reviewed in any orientation including orienting the epidermis at the top of dermatopathological slides; this was not possible in the past and was problematic when using slides for teaching.
- With suitable software, it is possible to incorporate annotations, such as circles and arrows, clinical photographs, images of dermoscopy or radiology, thereby making it ideal for teaching clinico-pathological correlation. By attaching a discussion, multimedia, web links and references, the usefulness of the images as teaching tools can be enhanced further.
- Whole slide imaging is useful for independent study (e-learning) and, with additional software, can provide instant real-time feedback, allowing participants to assess their own performance. Once the images and ancillary material are online, they can be accessed for review and further study at any time of day from anywhere and on any device.
- Whole slide imaging makes testing in pathology possible without the use of microscopes. In 2020, The American Board of Dermatology began using whole slide imaging exclusively in their board examinations. Microscopes and glass slides will no longer be used.
Continuing Medical Education and External Quality Assurance
Whole slide imaging is also useful in continuing medical education (CME) or continuing professional development (CPD) and external quality assurance (EQA). The incorporation of examinations with integrated multiple-choice questions makes it possible to accrue CME credit online. Accruing CME credit is becoming increasingly important for specialists. In some countries, it provides higher salaries, as is currently the case in Europe. In other countries, it is necessary for renewal of licensure and maintenance of speciality certification and is mandatory. The latter is already the case in the USA, along with mandatory certification examinations.
Digital pathology has been proven globally to be a strong tool for CME, CPD, and EQA-type programmes. Several key organisations, including the College of American Pathologists, the American Society for Clinical Pathology and the Royal College of Pathologists of Australasia, are already using digital pathology to deliver accredited CME exercises. In 2013-2015, the European Academy of Dermatology and Venereology offered their members a quarterly Clinico-Pathological Self-Assessment Module with whole slide imaging.
The American Society of Dermatopathology has an interactive case study of the month, which uses whole slide images with multiple choice answers and explanations: https://www.asdp.org/education/case-study-of-the-month/case-archive/
In addition, a number of pathology subspecialty EQA programmes in the UK use digital pathology.
Consultation and collaboration
Consultation between pathologists and clinicians around the globe is easily manageable. Suitable software allows the incorporation of the following with the slide data:
- Gross morphology
- Clinical photographs
- Dermoscopic images
- Radiological images
- Annotations
- Insertion of comments.
To view as an example of whole slide imaging, click on the sample dermatopathology image below.
Storage of scanned images for archiving, tumour boards and research
Some institutions use whole slide imaging for filing purposes.
- With increasing lack of storage space for histopathological slides, scanning pertinent slides and then discarding the original glass slides, while keeping the blocks, has become an option. This also reduces salary costs for employees, who no longer need to retrieve glass slides from storage.
- Storage of large banks, or software including digital slides, can be most easily achieved in data centers (cloud-based or local), and individual collections can be stored or backed up on hard drives.
- The digital slides are subsequently easily retrieved for use in research, or for tumour boards.
Inclusion in electronic medical records
- Digital pathology slides can be attached to the electronic medical records, making both consultation and transfer easily achievable.
Pattern recognition algorithms as a diagnostic tool
- Whole slide imaging enables manual and computer-assisted quantitative image analysis of diagnostic and prognostic protein and genetic biomarkers.
- The FDA recently approved the first AI algorithm in histopathology related to prostate Gleason grade. This has opened the door to many more approvals which are now in the pipeline.
Disadvantages of whole slide imaging
Disadvantages of whole slide imaging may include:
- Not all centres have histopathology slide scanners, although these are now becoming more common. Costs of high throughput scanners are still prohibitive, although they are becoming more affordable.
- Pathology WSI are huge files (250MB to 5GB); monthly storage and bandwidth costs charged by storage companies can be very high. On premises storage solutions are better, but need technical support and expertise.
- It is possible to send slides for scanning at commercial centres for a set fee.
- High-speed Internet connection is necessary to view large files (512 Kbps for the above image); this speed is now commonplace in developed countries.
- Digital slides scanned by different brands of scanners and software used for viewing the images may be incompatible. Current software can accommodate most types of digital slides, regardless of origin.
- Whole slide imaging software is expensive, as is managed hosting and service. Software lifetime may be limited.
Research into the validity of whole slide imaging
Studies of diagnostic accuracy using whole slide imaging have been done, comparing use of glass slides to digital slides as well as photomicrographs to digital slides. See references below. This is not a comprehensive list.