What is X-linked agammaglobulinaemia?
X-linked agammaglobulinaemia is an inherited genetic disorder characterised by the failure to produce mature B-lymphocytes and plasma cells. Affected patients have severe deficiencies in all immunoglobulins.
X-linked agammaglobulinaemia was first described in 1952 by Dr Ogden Bruton so is also called Bruton agammaglobulinaemia/hypogammaglobulinaemia.
What are gamma globulins?
Gamma globulins are also called immunoglobulins. They are proteins produced by plasma cells and are essential to the body’s immune defence system. Agammaglobulinaemia means the absence of gamma globulins.
Who gets X-linked agammaglobulinaemia?
The risk factors for X-linked agammaglobulinaemia include:
- Sex. The disease presents exclusively in males.
- Age. Patient generally begins to have symptoms between 6 and 18 months of age.
- Family history.
- Race. There appears to be no racial predilection.
What causes X-linked agammaglobulinaemia?
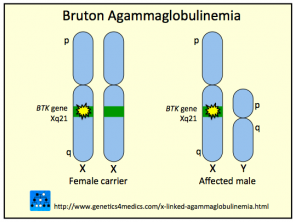
X-linked agammaglobulinaemia is caused by mutations on Bruton’s Tyrosine Kinase (BTK) gene, which was discovered in 1993. The gene normally promotes the maturation of B-lymphocytes. Since the BTK gene is found on the X-chromosome, X-linked agammaglobulinaemia presents exclusively in males. Females can present with an autosomal recessive version of agammaglobulinaemia.
Genetics of X-Linked-agammaglobulinemia
*Image courtesy Genetics 4 Medics
What are the clinical features of X-linked agammaglobulinaemia?
- Reduced lymphoid or reticuloendothelial organs, including the tonsil, lymph nodes, spleen, adenoids and intestinal Peyer patches
- Recurrent respiratory infections, including otitis media, pneumonia, bronchitis, or sinusitis; the most common causes are pneumococcus, streptococcus and staphylococcus.
- Chronic gastrointestinal symptoms eg, diarrhoea due to giardia infections
- Skin infections
Babies with X-linked agammaglobulinaemia appear healthy at first. They begin to have recurrent infections as the protection of their mother’s antibodies wears off.
How is X-linked agammaglobulinaemia diagnosed?
X-linked agammaglobulinaemia can be diagnosed on investigations including:
- Initial evaluation of serum immunoglobulins
- Measurement of B-cells in peripheral blood if initial testing reveals low serum immunoglobulins
- Molecular analysis, involving techniques such as single-strand confirmation polymorphism, DNA analysis, denaturing gradient gel electrophoresis, or reverse transcriptase polymerase tests on the BTK gene
- Genetic testing of the female relatives of a suspected X-linked agammaglobulinaemia patient
- In utero testing via chorionic villus sampling or amniocentesis
- Testing at birth for a decrease in CD19 B-cells, and an elevated level of T cells via fluorocytometric analysis.
What is the treatment for X-linked agammaglobulinaemia?
There is no cure for X-linked agammaglobulinaemia. However, treatment can greatly improve quality of life for X-linked agammaglobulinaemia patients.
- Life-long immunoglobulin replacement therapy, given intravenously or subcutaneously. This helps replace antibodies an X-linked agammaglobulinaemia patient cannot make for themselves.
- Antibiotics—sometimes used prophylactically to reduce infection rates.
- Avoid live vaccines—including measles, mumps, and rubella (MMR) vaccine, and the vaccines for polio, rotavirus, and varicella, which can cause the diseases they are supposed to prevent.
What is the outcome for X-linked agammaglobulinaemia?
Immunoglobulin replacement therapy reduces the risk of invasive infection. Chronic lung disease still develops and overall survival is reduced.