Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Author: Dr Kerry Gardner, Dermatology Registrar, Saskatchewan; Copy Editor: Clare Morrison; Chief Editor: Dr Amanda Oakley, Dermatologist, Hamilton, New Zealand; March 2014. Copy edited by Gus Mitchell.
Introduction Causes Demographics Clinical features Diagnosis Treatment Prognosis
Pretibial myxoedema is a form of diffuse mucinosis in which there is an accumulation of excess glycosaminoglycans in the dermis and subcutis of the skin. Glycosaminoglycans, also called mucopolysaccharides, are complex carbohydrates that are important for tissue hydration and lubrication. The main glycosaminoglycan in pretibial myxoedema is hyaluronic acid, which is made by cells called fibroblasts.
Pretibial myxoedema is also known as localised myxoedema, thyroid dermopathy, and infiltrative dermopathy.
It is most commonly seen on the shins (pretibial areas) and is characterised by swelling and lumpiness of the lower legs.
The exact mechanism for the deposition of glycosaminoglycans in the skin of the lower legs is uncertain.
Pretibial myxoedema is likely to be due to a combination of the following causes.
Pretibial myxoedema is nearly always associated with Graves disease. Graves disease is an autoimmune disorder that affects the thyroid gland in which there are antibodies to TSH-R activate the receptor, often causing an increase in circulating thyroid hormone. This is hyperthyroidism or thyrotoxicosis. Symptoms of thyrotoxicosis include weight loss, palpitations, sweating (hyperhidrosis), and tremors
The classic triad of signs of Graves disease is:
Pretibial myxoedema:

Pretibial myxoedema

Thyroid ophthalmopathy

Thyroid acropachy
Pretibial myxoedema can appear before, during, or after the thyrotoxic state. It is not related to thyroid function. It is generally seen 12–24 months after diagnosis.

Pretibial myxoedema in Graves disease

Pretibial myxoedema in Graves disease

Pretibial myxoedema in Graves disease
See more images of pretibial myxoedema ...
The types of pretibial myxoedema can include the following.
Diagnosis of pretibial myxoedema is made by taking a history and finding characteristic clinical appearance on examination of the patient.
Skin biopsy is rarely necessary for diagnosis, especially if there is a history of hyperthyroidism, or Graves ophthalmopathy.
If a biopsy is done, histopathology typically shows deposition of mucin (glycosaminoglycans) throughout the dermis and subcutis.
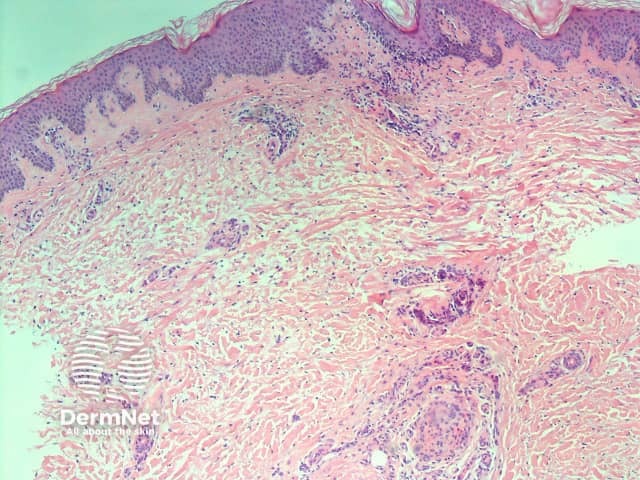
H&E stain
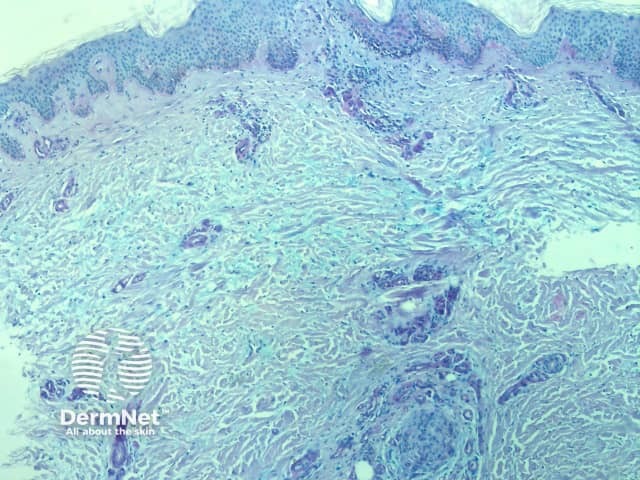
Positive mucin stain
Deposited mucin promotes dermal oedema by promoting the retention of fluid in the skin. This results in compression/occlusion of small peripheral lymphatics and lymphoedema.
The biopsy also shows attenuation of collagen fibres; they may be frayed, fragmented and widely separated. Stellate (star-shaped) fibroblasts are often observed, but the number of fibroblasts remains normal. Often a mild, superficial lymphocytic infiltrate around blood vessels is seen, and the overlying epidermis may show hyperkeratosis (increased scale).
Pretibial myxoedema is often asymptomatic and mild, and may require no treatment at all.
If symptomatic, treatment options include:
Other therapies reported to be successful include:
The prognosis is generally quite good. Most patients with asymptomatic pretibial myxoedema do not require treatment or follow-up.
The myxoedema clears up completely in the majority of patients with mild disease.
Even with more severe disease, it resolves in more than half of patients after several years. The elephantiasic form is the most difficult to treat, and is the least likely to clear up.
The likelihood of remission depends on the severity of the initial disease rather than its treatment.