Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Author: Anusha Preethi Panthagani, Dermatology Registrar, Royal Infirmary of Edinburgh, Scotland, United Kingdom; Chief Editor: Dr Amanda Oakley, Dermatologist, Hamilton, New Zealand, September 2015.
Introduction Causes Demographics Clinical features Diagnosis Treatment Outcome
Recessive X-linked ichthyosis is a genetic disorder in which there is very dry skin. The features include generalised, fine or rhomboid, adherent, dark brown or light grey, scaling of the skin. The scaling is usually prominent on the back of the neck, upper trunk and extensor surfaces of the limbs. The condition presents usually at birth or within 6 months of birth.
Recessive X-linked ichthyosis is associated with corneal opacities of the eye, undescended testicles and neurological abnormalities.
It is also sometimes just called X-linked ichthyosis.
Recessive X-linked ichthyosis is a disorder caused by a mutation of the enzyme steroid sulfatase (STS). STS is involved in the metabolism of cholesterol sulphate in the skin. STS deficiency leads to accumulation of cholesterol sulphate in the outer layer of the skin leading to a dysfunctional skin barrier and retention of the outer skin cells (corneocytes) causing the typical scaling.
The gene encoding STS has been mapped to the distal part of the X chromosome.
Therefore patients with X-linked ichthyosis should also be evaluated for the contiguous gene defect. Larger chromosomal deletions could result in:
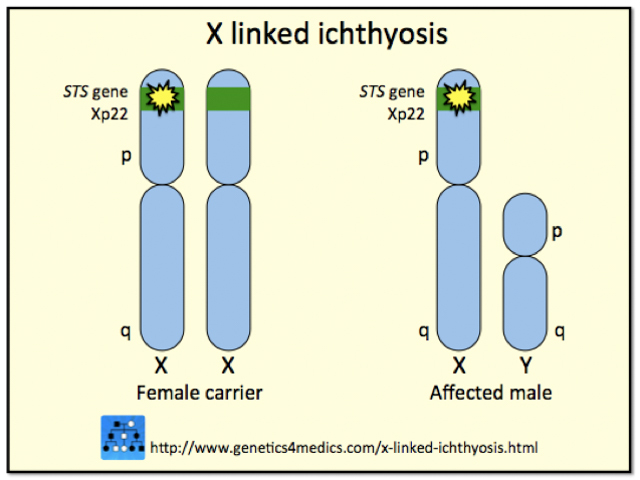
Genetics of X-linked ichthyosis*
*Image courtesy Genetics 4 Medics
The inheritance of X-linked ichthyosis is recessive because if the individual also has a normal STS gene, the condition is not expressed.
Females have two X-chromosomes and males have one. A male affected by X-linked ichthyosis passes the ichthyosis gene to his daughters via his X-chromosome. The daughters become carriers and usually have one affected gene and one normal gene. They can pass the abnormal gene to roughly half of their daughters and to half of their sons—who then manifest ichthyosis. Thus:
Approximately 1 in 6,000 males are affected by recessive X-linked ichthyosis, with no evident racial or geographical associations. There have been few cases reported in females. It is thought that these women have inherited the ichthyosis gene from both sides of the family.
Recessive X-linked ichthyosis presents with prominent scaling.

Recessive X-linked ichthysosis

Recessive X-linked ichthysosis

Recessive X-linked ichthysosis

Recessive X-linked ichthysosis

X linked ichthyosis

X linked ichthyosis
Non-skin manifestations of STS deficiency can occur as well.
Involvement of the adjacent genes in patients with recessive x-linked ichthyosis can result in a variety of additional features.
Diagnosis is based mainly on history and clinical findings.
Biochemical analysis after birth on the placenta, skin fibroblasts and keratinocytes includes:
Genetic analysis includes:
Genetic analyses have missed a few cases of x-linked ichthyosis caused by point mutations.
Pre-natal diagnostic tests for X-linked ichthyosis include:
Skin biopsy is usually not useful in confirming the disease as the epidermal microscopic findings may be subtle. They may include:
There is no definitive treatment for x-linked ichthyosis and current evidence is limited. High power studies for the treatments are lacking.
The aim of treatment is to improve the scaling of the skin and to improve the appearance of the skin. In some patients, treatment might not be required. Options include:
Genetic counselling can be also offered to patients and their families for further information regarding x-linked ichthyosis and inheritance pattern.
Research is ongoing to see whether patients can be treated with gene transfer.
Males should be advised to perform regular testicular self-examinations.
Recessive X-linked ichthyosis is a chronic condition and the disease persists through adult life.