What is urticaria?
Urticaria is characterised by weals (hives) or angioedema (swellings, in 10%) or both (in 40%). There are several types of urticaria. The name urticaria is derived from the common European stinging nettle 'Urtica dioica'.
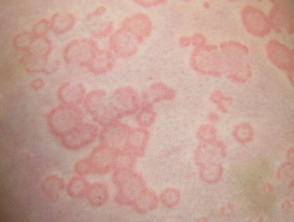
A weal (or wheal) is a superficial skin-coloured or pale skin swelling, usually surrounded by erythema (redness) that lasts anything from a few minutes to 24 hours. Usually very itchy, it may have a burning sensation.
Angioedema is deeper swelling within the skin or mucous membranes and can be skin-coloured or red. It resolves within 72 hours. Angioedema may be itchy or painful but is often asymptomatic.
Acute urticarial weals
What is acute urticaria?
Acute urticaria is urticaria, with or without angioedema, that is present for less than 6 weeks. It is often gone within hours to days.
Who gets acute urticaria?
One in five children or adults has an episode of acute urticaria during their lifetime. It is more common in atopic individuals. It affects all races and both sexes.
What causes acute urticaria?
Weals are due to release of chemical mediators from tissue mast cells and circulating basophils. These chemical mediators include histamine, platelet-activating factor and cytokines. The mediators activate sensory nerves and cause dilation of blood vessels and leakage of fluid into surrounding tissues. Bradykinin release causes angioedema.
Several hypotheses have been proposed to explain urticaria. The immune, arachidonic acid and coagulation systems are involved, and genetic mutations are under investigation.
Serum sickness and serum sickness-like reactions are due to immune complex deposition in affected tissues.
Acute urticaria can be induced by the following factors but the cause is not always identified.
- Acute viral infection — an upper respiratory infection, viral hepatitis, infectious mononucleosis
- Acute bacterial infection — a dental abscess, sinusitis, mycoplasma
- Food allergy (IgE mediated) — usually milk, egg, peanut, shellfish
- Drug-induced urticaria (IgE mediated) — often an antibiotic
- Drug-induced urticaria due to pseudoallergy — aspirin, nonselective nonsteroidal anti-inflammatory drugs, opiates, radiocontrast media; these cause urticaria without immune activation
- Vaccination
- Bee or wasp stings
- Widespread reaction following localised contact urticaria — rubber latex
Severe allergic urticaria may lead to anaphylactic shock (bronchospasm, collapse).
A single episode or recurrent episodes of angioedema without urticaria can be due to an angiotensin-converting enzyme (ACE) inhibitor drug.
What are the clinical features of acute urticaria?
Urticarial weals can be a few millimetres or several centimetres in diameter, coloured white or red, with or without a red flare. Each weal may last a few minutes or several hours and may change shape. Weals may be round, or form rings, a map-like pattern, targetoid lesions, or giant patches.
Acute urticaria can affect any site of the body and tends to be distributed widely.
Angioedema is more often localised. It commonly affects the face (especially eyelids and perioral sites), hands, feet and genitalia. It may involve tongue, uvula, soft palate, larynx.
Serum sickness due to blood transfusion and serum sickness-like reactions due to certain drugs cause acute urticaria leaving bruises, fever, swollen lymph glands, joint pain and swelling.
Urticaria and angioedema
How is acute urticaria diagnosed?
Acute urticaria is diagnosed in people with a short history of weals that last less than 24 hours, with or without angioedema. A thorough physical examination should be undertaken to look for underlying causes.
Skin prick tests and radioallergosorbent tests (RAST) or CAP fluoroimmunoassay may be requested if a drug or food allergy is suspected in acute urticaria.
Biopsy of urticaria can be non-specific and difficult to interpret. The pathology shows oedema in the dermis and dilated blood vessels, with a variable mixed inflammatory infiltrate. Vessel-wall damage indicates urticarial vasculitis.
What is the treatment for acute urticaria?
The main treatment for acute urticaria in adults and in children is with an oral second-generation antihistamine chosen from the list below. If the standard dose (eg 10 mg for cetirizine) is not effective, the dose can be increased fourfold (eg 40 mg cetirizine daily). They are best taken continuously rather than on demand. They are stopped when the acute urticaria has settled down. There is not thought to be any benefit from adding a second antihistamine.
- Cetirizine
- Loratadine
- Fexofenadine
- Desloratadine
- Levocetirizine
- Rupatadine
- Bilastine
Terfenadine and astemizole should not be used as they are cardiotoxic in combination with ketoconazole or erythromycin. They are no longer available in New Zealand.
Although systemic treatment is best avoided during pregnancy and breastfeeding, there have been no reports that second-generation antihistamines cause birth defects. If treatment is required, loratadine and cetirizine are currently preferred.
Conventional first-generation antihistamines such as promethazine or chlorpheniramine are no longer recommended for urticaria.
Psychotherapy is reported to benefit some patients with chronic urticaria.
Avoidance of trigger factors
In addition to antihistamines, the cause of urticaria should be eliminated if known (eg drug or food allergy). Avoidance of relevant type 1 (IgE-mediated) allergens clears urticaria within 48 hours.
In addition to antihistamines, the triggers for urticaria should be avoided where possible. For example:
- Avoid aspirin, opiates and nonsteroidal anti-inflammatory drugs (paracetamol is generally safe).
- Avoid known allergies that have been confirmed by positive specific IgE/skin prick tests if these have clinical relevance for urticaria.
- Cool the affected area with a fan, cold flannel, ice pack or soothing moisturising lotion.
Treatment of refractory acute urticaria
If non-sedating antihistamines are not effective, a 4 to 5-day course of oral prednisone (prednisolone) may be warranted in severe acute urticaria, particularly if there is angioedema. Systemic steroids do not speed up the resolution of symptoms.
Intramuscular injection of adrenaline (epinephrine) is reserved for life-threatening anaphylaxis or swelling of the throat.