Oral hairy leukoplakia is caused by Epstein-Barr virus (EBV) infection of the oral mucosa. It most often occurs in association with HIV infection. It has been less frequently described in immunosuppressed patients, especially following organ transplantation, and is rare in immune competent individuals.
Histology of oral hairy leukoplakia
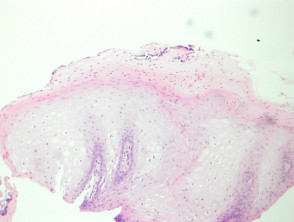
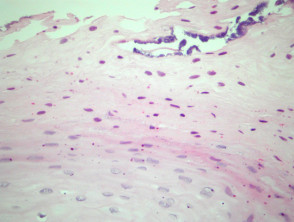
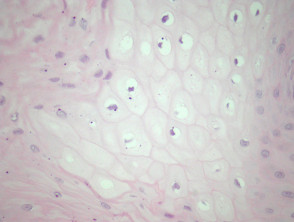
In oral hairy leukoplakia, the mucosa displays mild papillary acanthosis (figure 1). Hyperkeratosis and marked parakeratosis of the superficial epithelial layer is a prominent feature (figure 2). Superficial infections of the hyperkeratinized epithelium with bacteria or Candida may also be seen. The acanthosis is caused by ballooning koilocyte-like cells. (Figures 1, 3). The nuclei of these have a homogenous ground-glass appearance and may contain intranuclear inclusions.
Oral hairy leukoplakia pathology
Special studies for oral hairy leukoplakia
Diagnosis requires demonstration of EBV DNA, RNA, or protein within the epithelial cells of the lesion. In-situ hybridisation for EBV is usually performed for confirmation of the diagnosis.
Differential diagnosis of oral hairy leukoplakia
Oral candidiasis: Oral hairy leukoplakia is often colonised by candida which can obfuscate the pathology
Human papillomavirus (HPV): The koilocyte-like cells in oral hairy leukoplakia resemble HPV infection. In-situ hybridisation for EBV distinguishes these entities.