What is dermatomyositis?
Dermatomyositis is an idiopathic inflammatory myopathy characterised by skeletal muscle weakness and skin changes.
Who gets dermatomyositis?
Dermatomyositis is uncommon, with an annual incidence of 0.1-6 per population of 100,000. It can affect people of any race, age, and sex; however, women are affected twice as often as men, and Black Americans are more commonly affected than white Americans. It can present in children (see Juvenile dermatomyositis). The peak age group affected in adults is those aged 50–60 years.
Adult-onset dermatomyositis is strongly associated with malignancy; up to 25% of affected adults have an unknown underlying malignancy on diagnosis. The majority are adenocarcinomas.
What causes dermatomyositis in adults?
Dermatomyositis is thought to be caused by a microangiopathy affecting skin and muscle. There is a genetic predisposition to the development of dermatomyositis such as the PTPN22 gene and HLA associations identified include:
- Caucasian populations: HLA DRB1*0301 and DQA1*0501
- Asian populations: HLA-B7
- Anti-Jo-1 antibodies: HLA DRB1*0301 and DQA1*501
- Anti-Mi-2 antibodies: HLA DRB1*07 and DQA*0201.
Triggers and reported associations have included:
- Medications — see Drug-induced dermatomyositis
- Malignancy
- Viral infections — enteroviruses, parvovirus B19, influenza
- Silica exposure — in tradespeople.
Most patients have disease-associated autoantibodies, suggesting dermatomyositis is an autoimmune condition.
What are the clinical features of adult-onset dermatomyositis?
The skin changes of dermatomyositis will often, but not always, precede the muscle weakness. A face rash is the commonest initial skin sign, typically followed by scalp symptoms then the changes on the hands.
Cutaneous features of dermatomyositis
Characteristic skin changes of dermatomyositis include:
- Heliotrope rash — bilateral lilac discolouration of the eyelids (particularly the upper eyelids) with swelling of the eyelids and skin around the eyes
Heliotrope rash of dermatomyositis
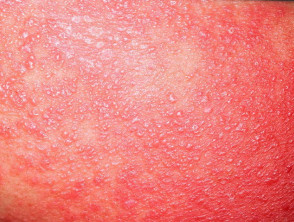
- Shawl sign — fixed redness affecting the back, shoulders, chest, and neck which can become poikilodermatous
Shawl sign of dermatomyositis
- Photosensitivity — sunburn reaction over the ‘V’ area of the anterior chest, face, and other sun-exposed sites
Photosensitivity of dermatomyositis
- Gottron papules — purple papules and plaques over the tops of the small joints of the hands
Gottron papules of dermatomyositis
- Gottron sign — redness over the backs of the hands, elbows, and knees
Gottron sign of dermatomyositis
- Scalp involvement — itchy scaly scalp with inflammation and diffuse, non-scarring thinning of the hair, and sometimes poikiloderma
Scalp involvement in dermatomyositis
- Nailfold changes — ragged cuticles and red nailfolds; dermoscopy demonstrates prominent blood vessels in the proximal nailfolds
Nailfold changes in dermatomyositis
- Flagellate erythema
- Holster sign – redness over the buttocks and lateral thighs
- Mechanic’s hands — hyperkeratotic changes seen in antisynthetase syndrome
- Vesicles and bullae (blisters)
- Raynaud phenomenon
- Calcinosis cutis — uncommon in adult-onset dermatomyositis (10%).
Calcinosis cutis and Raynaud phenomenon
Myositis of dermatomyositis
Muscle weakness may appear at the same time as the skin rashes, or it may occur weeks, months, or even years later. Amyopathic dermatomyositis presents with only skin changes and no clinical evidence of myositis, although this is usually found on investigation. The myositis usually affects the proximal muscles, those closest to the trunk as in the upper arms and thighs. The first indication of myositis is when the following every day movements become difficult with weakness and fatigue:
- Climbing stairs or walking
- Rising from a sitting or crouching position
- Lifting objects
- Raising arms above the shoulders, such as when combing hair
- Difficulty swallowing.
The muscles may ache and become tender to touch.
How do clinical features vary in differing types of skin?
The heliotrope rash around the eyes characteristic of dermatomyositis can be difficult to distinguish in dark skin. Other clinical signs may be required to suggest the diagnosis.
Dermatomyositis in skin of colour
What are the complications of adult-onset dermatomyositis?
When dermatomyositis affects swallowing, it may be complicated by:
- Weight loss
- Aspiration pneumonia.
Other systemic features of dermatomyositis may include:
- Arthritis
- Cardiac arrhythmias
- Interstitial lung disease
- Pulmonary arterial hypertension.
How is adult-onset dermatomyositis diagnosed?
The diagnosis of dermatomyositis is suggested by the clinical features, and confirmed on investigations.
A skin biopsy of the rash shows an interface dermatitis similar to cutaneous lupus erythematosus, so histology alone cannot be used to distinguish the two conditions. Dermoscopy or trichoscopy may also be used for closer inspection.
Blood tests assess the myositis and autoantibody subsets.
- Muscle enzymes — creatine kinase (CK), aldolase, aspartate aminotransferase (AST) and lactic dehydrogenase (LH).
- Anti-aminoacyl-transfer RNA synthetase antibodies — anti-Jo-1, anti-OJ, anti-EJ, anti-KS, anti-Zo, anti-Ha, anti-PL-1 are associated with antisynthetase syndrome.
- Anti Mi-2 is associated with disease mainly affecting the skin.
- Anti-transcriptional intermediary factor 1y antibodies (TIF-1y, anti 155/140) are strongly associated with malignancy-related dermatomyositis in the elderly.
- Anti-melanocyte differentiation-associated protein 5 (anti-MDA5) is associated with rapidly progressive interstitial lung disease and skin ulcers.
- Anti-NXP2 (MJ) antibody is associated with pronounced muscle symptoms and less with skin changes.
Further investigation of the muscle disease may require:
- Electromyography (EMG)
- Muscle biopsy
- Magnetic resonance imaging (MRI).
Age-appropriate investigations for an underlying malignancy should be considered after careful history and general examination.
What is the differential diagnosis for adult-onset dermatomyositis?
Dermatomyositis may need to be distinguished from:
- Other idiopathic inflammatory myopathies, such as polymyositis or inclusion body myositis
- Systemic lupus erythematosus (SLE) and other connective tissue diseases.
What is the treatment for adult-onset dermatomyositis?
General measures
General measures for the treatment of dermatomyositis include:
- Photoprotection and sun-avoidance
- Bedrest
- Physical therapy and activity
- Elevating the bedhead for those with difficulty swallowing.
Specific measures
Measures for more specific treatment of dermatomyositis can include:
- Topical steroids
- Topical calcineurin inhibitors
- Systemic corticosteroid such as prednis(ol)one
- Hydroxychloroquine, although cutaneous adverse effects are more common in dermatomyositis than in SLE
- Intravenous immunoglobulin (IVIG), FDA-approved in 2021
- Steroid-sparing agents and other immunosuppressants, including:
- Diltiazem and colchicine may reduce calcinosis.
The JAK inhibitor, baricitinib, was studied in a small, 12-patient, open-label trial with clinically significant improvement seen in as early as week 4 of the study. Apremilast was also studied in 8 adult women as add-on therapy with positive results.
What is the outcome for adult-onset dermatomyositis?
Dermatomyositis may resolve in 20% of adults who have the condition, but most will require lifelong treatment. The prognosis of those with associated conditions such as malignancy, heart or lung involvement will be impacted and may be life-shortening.