Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Introduction - aspergillosis Introduction - aspergillus Demographics Causes Clinical features Skin manifestations Diagnosis Treatment Prevention
Aspergillosis is disease caused by aspergillus.
Aspergillus is a fungus (mould) that is found in abundance throughout the environment in soil, decomposing plant matter, ornamental plants, water, household dust, and building materials. More than 100 different species of aspergillus have been identified, but the species most commonly implicated in human disease are A. fumigatus, A. flavus, and A. niger.
Aspergillosis is more frequently diagnosed when conditions producing impaired immunity become more prevalent. For example, invasive aspergillosis is estimated to occur in 5–13% of recipients of bone marrow transplants, in 5–25% of patients who have received heart or lung transplants, and in 10–20% of patients who are receiving intensive chemotherapy for leukaemia.
The term aspergillosis is not used to refer to chronic nail infections caused by aspergillus, which is a form of onychomycosis that affects people with normal immune systems.
Aspergillus most commonly enters the human body via inhalation. Most people breathe in aspergillus spores every day, with no ill-effect. However, in patients with pre-existing medical conditions, aspergillus can start to proliferate and cause disease, primarily a lung infection. Infection is more likely if a large number of spores are inhaled, such as on exposure to a very dusty environment or during renovation of a building.
On rare occasions, the fungus may enter via the skin (primary cutaneous aspergillosis), particularly in patients with thermal burns or trauma. Occasionally, outbreaks of primary cutaneous aspergillosis is due to contaminated biomedical equipment.
Aspergillus can also spread to the skin via the blood stream.
There are four common clinical patterns of disease.
Acute invasive apsergillus affects people with severely impaired immunity, particularly those:
Allergic aspergillosis can affect anyone, but is more common in people with asthma or cystic fibrosis.
Aspergilloma affects people with an underlying cavity-causing lung disease, such as tuberculosis, emphysema, or cystic fibrosis.
Skin changes are most commonly a consequence of widespread infection with aspergillus in patients with impaired immunity.
Primary cutaneous aspergillosis most commonly develops at the site of an intravenous cannula insertion or venipuncture (wound from a blood test).

Aspergillus skin lesion

Cutaneous aspergillosis

Cutaneous aspergillosis
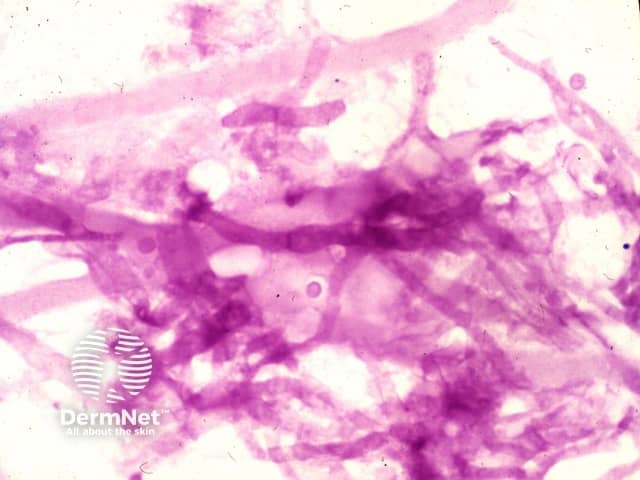
Potassium hydroxide of culture
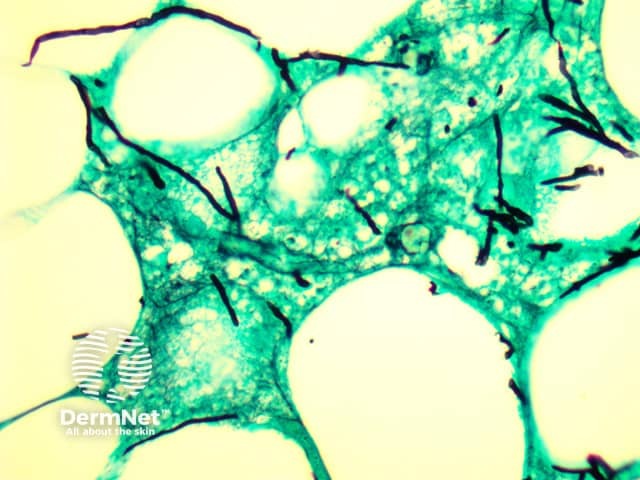
Histopathology
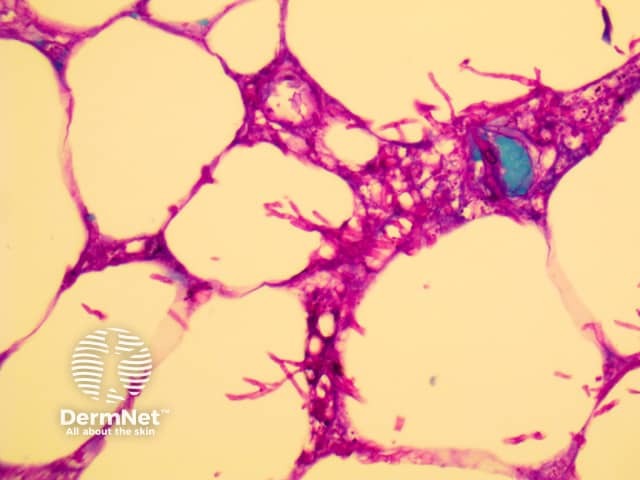
Histopathology
Because the aspergillus fungus is present everywhere throughout the environment, it is virtually impossible to avoid it altogether. In patients with severely impaired immunity, the following measures may be helpful: