What is dermatitis herpetiformis?
Dermatitis herpetiformis (DH) is an inflammatory immunobullous disease of the skin and a cutaneous manifestation of coeliac (celiac) disease, a gluten-sensitive enteropathy.
The name herpetiformis is derived from the tendency for blisters to appear in clusters, resembling herpes simplex. However, DH is not due to viral infection.
DH is also known as Duhring-Brocq disease.
Clustered vesicles have been excoriated on the elbows in dermatitis herpetiformis
Elbow, sacral and buttock lesions - the classical distribution of dermatitis herpetiformis
Excoriated vesicles on the buttocks and sacrum in dermatitis herpetiformis Dermatitis herpetiformis
Hairline lesions in dermatitis herpetiformis
Dermatitis herpetiformis





More images of dermatitis herpetiformis
Who gets dermatitis herpetiformis?
- Dermatitis herpetiformis (DH) has a prevalence of 10 per 100,000 population.
- DH predominantly affects Caucasians aged 15–50 years, but may occur in other ages and ethnicities.
- It is rare in those of African and Asian ancestry, and most common in Irish and Swedish people.
- Mean age at diagnosis is 40–50 years.
- There is a male predominance of 2:1.
- More females <20 years are affected than males; males tend to present at a later age.
- There is a genetic predisposition with an association with human leukocyte antigens (HLA) DQ2 and DQ8. ~90% of patients with coeliac disease carry HLA-DQ2, leaving only a small proportion of patients with lower risk heterodimers (such as HLA-DQ8). 10–15% of individuals with DH have an affected first degree relative.
- Some patients have a personal or family history of other autoimmune diseases including thyroid disease, pernicious anaemia, type 1 diabetes, vitiligo, Addison disease, alopecia areata, and haemochromatosis.
What causes dermatitis herpetiformis?
- Dermatitis herpetiformis (DH) and coeliac disease are due to intolerance to the gliadin fraction of gluten found in wheat, rye, and barley.
- Gluten triggers production of IgA antibodies and an autoimmune process that targets the skin and gut.
- In coeliac disease, gluten causes intestinal inflammation resulting in diarrhoea, tiredness, weight loss, abdominal discomfort, and metabolic consequences of malabsorption.
- The majority (>90%) of patients with DH also have gluten-sensitive enteropathy. Gastrointestinal symptoms are usually mild; some patients remain symptom-free.
- Around 15–25% of coeliac patients have concurrent DH. These patients tend to have a more severe intestinal pathology in comparison to those without DH.
What are the clinical features of dermatitis herpetiformis?
DH presents as intense itch and a symmetrical blistering rash. Vesicles (often 3–5 mm in diameter) or blisters develop on erythematous skin but are often eroded and crusted due to scratching.
- Distribution is a helpful diagnostic clue; lesions most commonly appear on the scalp, shoulders, buttocks, elbows, and knees.
- It is characterised by prurigo (extremely itchy papules) and vesicles on normal or reddened skin.
- DH may also present initially as digital petechiae.
- Flat red patches, thickened plaques, and weals may occur resembling other inflammatory skin conditions such as dermatitis, scabies, and papular urticaria.
- Lesions resolve to leave postinflammatory hypopigmentation and hyperpigmentation.
DH may be exacerbated by some medications (eg, potassium iodide, non-steroidal anti-inflammatory medications, leuprolide acetate, progesterone), and premenstrually.
Images of dermatitis herpetiformis
How does dermatitis herpetiformis differ in skin of colour?
While uncommon, clinical features are similar, although postinflammatory pigmentation is more prominent.
What are the complications of dermatitis herpetiformis and coeliac disease?
The following conditions may affect patients with dermatitis herpetiformis (DH), especially when it is associated with coeliac disease:
- Aphthous ulcers and angular cheilitis
- Dry skin, nail, and hair abnormalities
- Dental problems: thin enamel
- Neurological problems: ataxia (loss of balance), polyneuropathy, epilepsy
- Heart problems: pericarditis and cardiomyopathy
- Recurrent miscarriages
- Fatty liver resulting in abnormal liver function tests
- Non-Hodgkin lymphoma (NHL)* affecting the intestines or any part of the body.
*The risk of NHL is increased six to tenfold among DH patients. Strict adherence to a gluten-free diet reduces this rare but serious complication. Fortunately, increased lymphoma risk is evident only during the first 5 years after DH diagnosis and gluten-free diet adherence.
How is dermatitis herpetiformis diagnosed?
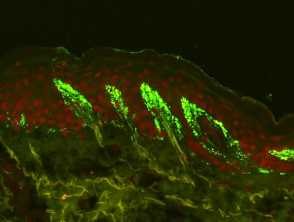
Skin biopsy is usually necessary to confirm DH.
Lesional skin may show:
- Subepidermal blisters
- Neutrophil and eosinophil inflammatory cells in the dermal papillae.
Uninvolved perilesional skin contains a significantly greater number of IgA deposits, and lesional biopsies in general have a higher false negative rate.
- DH is characterised by granular deposits of IgA at the dermoepidermal junction papillae.
- Perilesional skin biopsy using direct immunofluorescence is the gold standard test for diagnosis of DH (90–95% sensitivity; 95–100% specificity).
See Dermatitis herpetiformis pathology for more information.
Screen for nutritional deficiencies
Patients with DH are commonly offered the same blood tests used for patients with coeliac disease to screen for nutritional deficiencies. These include:
- Full blood count, liver function tests, and serum calcium
- Iron, ferritin, zinc, vitamin B12, and folate
- Thyroid function tests.
Mild anaemia may be caused by iron or folic acid deficiency (or both) due to malabsorption associated with gluten-sensitive enteropathy. Thyroid function tests are usually recommended due to the association between DH and thyroid disease.
Diagnostic blood tests
Specific autoantibody tests for DH are:
- IgA anti-endomysial antibodies (present in 80% of patients with DH)
- IgA tissue transglutaminase antibody (tTG)
- IgA epidermal transglutaminase antibodies (eTG), when available
- DH is associated with IgA eTG, which is not the case in coeliac disease
- IgA and IgG deamidated gliadin peptide antibody (dGP)
- IgA and IgG gliadin assay
- Total IgA level.
Borderline results may be difficult to interpret.
Small intestinal biopsy
DH patients with abnormal blood results usually proceed to have a small intestinal biopsy to confirm gluten-sensitive enteropathy. This is histologically characterised by small bowel villous atrophy. This means that instead of being highly convoluted, the lining of the intestines is smooth and flattened.
The small bowel may appear normal because of treatment (gluten-free diet and/or medication), skip lesions (the sample was taken from an unaffected site), or the intestine may be unaffected by the disease.
Other tests
HLA haplotype testing (for a set of DNA variations) may reveal HLA-DQ2 or HLA-DQ8. This is present in almost all patients with DH (and coeliac disease).
What is the differential diagnosis of dermatitis herpetiformis?
- Linear IgA bullous disease
- Bullous pemphigoid
- Atopic dermatitis/eczema
- Scabies
- Papular urticaria
- Prurigo nodularis/nodular prurigo
What is the treatment for dermatitis herpetiformis?
Gluten-free diet
A gluten-free diet for life is strongly recommended in patients with DH, as it:
- Reduces the requirement for medication to control DH
- Improves associated gluten-sensitive enteropathy
- Enhances nutrition and bone density
- May reduce the risk of developing other autoimmune conditions
- May reduce the risk of intestinal lymphoma.
It may take up to 2 years for a gluten-free diet to reach its maximal effect.
Medication
Dapsone is the treatment of choice for DH, as it usually reduces itch within 3 days.
- Dose ranges from 25–300 mg daily.
- It may be gradually weaned off in those who have been on a stable gluten-free diet.
- The effects of dapsone are seen rapidly. Symptoms of itch resolve within several hours and new blister formation ceases in 24–36 hours. It is an effective option in the early stages of gluten-free diet initiation.
- Dapsone has no effect on enteropathy, deposition of IgA antibodies, or lymphoma risk.
- Dapsone has potential side effects and monitoring requirements.
- Agranulocytosis (occurring 3–12 weeks after initiation), dapsone hypersensitivity (usually 4–6 weeks after initiating treatment), and methaemaglobinopathy are rare but serious complications. Dapsone must be stopped immediately in these scenarios.
If intolerant or allergic to dapsone, the following may be useful:
- Ultra-potent topical steroids
- Systemic steroids
- Colchicine
- Ciclosporin
- Azathioprine
- Sulfapyridine
- Rituximab.
There are reports that combination therapy with dapsone and sulfasalazine may be effective in patients who do not tolerate increasing doses of dapsone monotherapy.
Topical dapsone 5% gel was also shown to be effective as an adjuvant treatment for DH. Compared to oral dapsone, topical dapsone was associated with a lower incidence of side effects and can be administered safely in patients with glucose-6-phosphate dehydrogenase (G6PD) deficiency.
What is the outcome for dermatitis herpetiformis?
Dermatitis herpetiformis usually has a good prognosis, with the majority of patients responding well to a strict gluten-free diet and medication. A lifelong gluten-free diet is required. Although the overall incidence of T cell lymphoma is increased in DH, the overall disease mortality is lower than the general population, possibly due to a reduction in cardiovascular disease and obesity.