What is eosinophilic fasciitis?
Eosinophilic fasciitis, also called Shulman syndrome, is a rare variant of scleroderma or deep form of morphoea involving the subcutis and fascia of the skin characterised by fascial thickening with an eosinophilic tissue infiltrate and peripheral eosinophilia.
Eosinophilic fasciitis
Who gets eosinophilic fasciitis?
Eosinophilic fasciitis usually affects adults aged 20–60 years, although there are reports in children and the elderly. Both sexes can be affected, with a slight male predominance (1.5:1). Occurrence in siblings has been reported but it is not regarded as an inherited condition. It may predominantly affect Caucasians, although there are cases reported from Japan, India, and other patients with skin of colour.
What causes eosinophilic fasciitis?
Eosinophilic fasciitis is possibly the result of an autoimmune mechanism targeting damaged fascia. Autoantibodies including rheumatoid factor (RF) and antinuclear antibodies (ANA) are sometimes detected.
Eosinophils may release transforming growth factor (TGF) beta to activate fibroblasts resulting in increased expression of type I collagen, fibronectin, and tissue inhibitor of metalloproteinase-1 (TMIP-1) resulting in fibrosis.
Triggers for developing eosinophilic fasciitis include:
- Unusually vigorous activity — most common aetiological factor reported in 50%
- Insect bites
- Radiation therapy
- Infections — Mycoplasma arginini, Borrelia burgdorferi
- Medications — atorvastatin, carbidopa, immune checkpoint inhibitors (eg, pembrolizumab, nivolumab)
- Paraneoplastic (5–10%) — usually haematolymphoid (eg, leukaemias, myeloproliferative disorders) rather than solid tumours
- Chronic graft-versus-host disease.
What are the clinical features of eosinophilic fasciitis?
Eosinophilic fasciitis typically develops suddenly 1–2 weeks after strenuous exercise or work; less commonly the onset is gradual.
- Painful, red forearms and lower legs with pitting oedema
- Symmetrical full-circumference involvement, rarely unilateral
- Skin becomes uneven, resembling the skin surface of an orange (peau d’orange) due to fibrosis and prominent hair follicles
- Woody induration and plate-like hardness gradually develops
- Groove Sign — linear furrows overlying superficial veins emphasised by elevation of the limb
- Spares face, hands, and feet, may involve thighs and upper arms
- Common systemic symptoms include fever, fatigue, myalgia, arthralgia, and weight loss
- Lack of Raynaud phenomenon, sclerodactyly, nailfold telangiectases, or internal organ involvement
Skin signs of eosinophilic fasciitis
Image of groove sign in eosinophilic fasciitis: Oliveira M, Patinha F, Marinho A. Eosinophilic fasciitis after parasite infection. Reumatologia. 2016;54(1):38-41. doi:10.5114/reum.2016.58761 Journal
Image of peau d'orange in eosinophilic fasciitis: Adachi Y, Mizutani Y, Shu E, Kanoh H, Miyazaki T, Seishima M. Eosinophilic fasciitis associated with myositis. Case Rep Dermatol. 2015;7(1):79-83. doi:10.1159/000381845 Journal
What are the complications of eosinophilic fasciitis?
- Joint contractures restrict the range of movement
- Symmetrical non-erosive arthritis
- Carpal tunnel syndrome due to pressure on the median nerve
- Other compartment syndromes
How is eosinophilic fasciitis diagnosed?
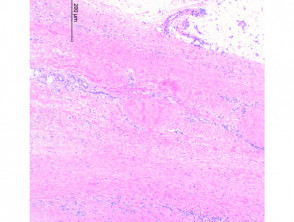
Eosinophilic fasciitis should be considered on the typical history and examination, and confirmed on deep skin biopsy including subcutis, fascia, and muscle [see Eosinophilic fasciitis pathology].
Diagnosis of eosinophilic fasciitis requires the major criterion and one or both of the two minor criteria:
- Major criterion — symmetrical plate-like sclerotic lesions on all four limbs
- Minor criteria
- Skin biopsy shows fibrosis of the subcutaneous connective tissue, thickening of the fascia, and infiltrate of eosinophils and monocytes
- Thickening of the fascia seen on imaging such as MRI or PET
Blood tests in early active disease:
- Peripheral eosinophilia — may be transient
- Elevated ESR and C-reactive protein (CRP)
- Hypergammaglobulinaemia — polyclonal, detected in 60%
- Elevated serum aldolase
- Serum type III procollagen peptide (PIIIP) — level reflects disease activity
- ANA and RF — positive in 10%.
What is the differential diagnosis for eosinophilic fasciitis?
- Morphoea (localised scleroderma) and systemic sclerosis
- Hypereosinophilic syndrome
- Nephrogenic fibrosing nephropathy
Differential diagnosis of eosinophilic fasciitis
What is the treatment for eosinophilic fasciitis?
- Pulse or oral corticosteroids — eg, methylprednisolone, prednisolone
- Phototherapy — UVA1, PUVA
- Other immunosuppressive systemic treatments — eg, ciclosporin, methotrexate
- Biological treatments — eg, infliximab, rituximab
- Physiotherapy
What is the outcome for eosinophilic fasciitis?
Eosinophilic fasciitis can be associated with or progress to morphoea or other autoimmune connective tissue disorders in 20–30% of cases. Associated haematological disorders such as aplastic anaemia and lymphoma have been reported.
Spontaneous recovery is reported in 10–20% after 2–5 years. Treatment is typically required for months to years. The prognosis for survival is good; joint contractures and skin hardness may persist if treatment is delayed.