The aims of wound closure
Surgical wounds can be left to heal by themselves (secondary intention healing), or they can be closed surgically. Secondary intention can take weeks to months depending on the size and location. Ultimately a relatively broad contracted scar is formed. Secondary intention healing may, however, be preferred over surgical closure in the following situations:
- Contaminated wounds, as the risk of an infection is higher when these wounds are sutured
- Wounds in concave sites such as parts of the ear or medial canthus
- If surgical reconstruction requires a larger reconstruction than desired or if the patient is unfit for such surgery
Reasons to choose a surgical type of wound closure instead can be to:
- Speed up the wound closure
- Protect underlying tissues (eg, bone, cartilage, nerve)
- Improve function by choosing the direction of skin tension on the wound edges (eg, avoiding ectropion)
- Improve cosmesis by hiding the scar on borders of cosmetic (sub) units as much as possible
Surgical techniques to close a wound include:
Primary closure
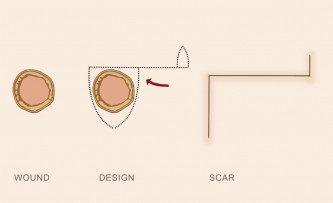
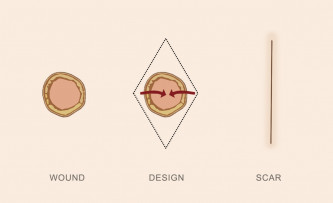
Primary closure refers to direct apposition of wound edges. See schematic diagram of primary closure design.
1. The edges of the wound may be undermined to free up the wound edges and reduce tension.
2. Sutures are then placed to close the wound.
3. It is often preferable to place two layers of sutures: one layer of dissolving sutures buried in the dermis or deeper tissue layers, followed by either dissolving or non-dissolving sutures under minimal tension to neatly oppose the epidermis.
4. For high tension wounds or wounds on fragile skin, special suture techniques may be used to spread tension along the wound edge.
Skin flap
Skin flap refers to a procedure where tissue is moved or lifted from a donor site to cover the recipient site (the wound) while leaving the blood supply intact. For each type of flap, a basic diagram explaining the design is included.
Advancement flap
An incision from the wound edge towards the side of the wound is made. The area of adjacent skin is undermined and advanced laterally to approximate wound edges. Excess skin at the end of the incision needs to be addressed by excising it ("dog-ear correction"), as shown in the drawing, or with a Z-plasty.
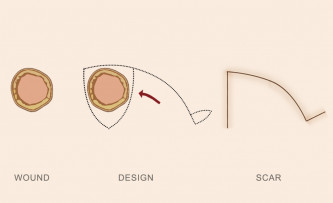
Rotation flap
A semicircular incision is made starting at the wound edge. The area of adjacent skin is undermined and advanced towards the wound edges by rotating it. Similar to the advancement flap, it is usually required to adjust for excess skin at the end of the incision. Rotation and advancement flaps are similar in design and often overlap.
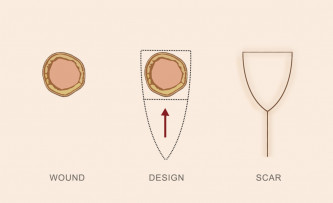
Island pedicle flap
Also referred to as a V-Y flap. A V-shaped incision is made, after which the area underneath this is undermined leaving a subcutaneous pedicle intact for blood supply. This results in a piece of pedicled skin (the island) that can be freely moved toward the wound edge, creating a Y-shaped scar.
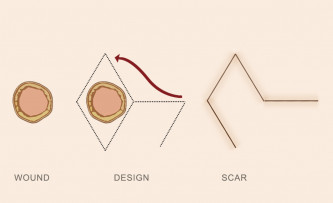
Transposition flap
This type of flap involves lifting tissue into the defect over the top of the intact surrounding skin. One of the basic types of transposition flaps is a rhomboid flap, the design of which is shown in the schematic drawing. When the donor site is too far away from the recipient site (the wound), a vascular pedicle can be left intact that is also transposed over or under an area of normal skin forming a bridge or tunnel. This is called an interpolation flap. The pedicle is divided at a later stage when new blood supply at the donor site has been formed. Common examples of this type of flap are the paramedian forehead, melolebial and retroauricular flaps.
Free flap
Tissue from a distant site is cut loose from the donor site and reattached to the vasculature of the recipient site.
Skin graft
A skin graft refers to a procedure where the skin is completely excised from another site and sewn into the defect to patch the wound. The graft is dependent on local oxygen supply at the donor site and therefore requires a well-vascularised wound bed. There are different types of skin grafts.
- Full-thickness skin graft. A piece of skin is excised down to the level of fat and therefore includes epidermis and the full thickness of the dermis and adnexal structures such as hair follicles.
- Split-thickness skin graft. Skin is excised to the level of superficial to the mid dermis.
- Composite graft. Contains full-thickness skin and underlying tissue (eg, muscle, fascia, cartilage).