Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Lesions (cancerous) Diagnosis and testing
Author: Qiuyu Jin, Medical Student, University of Auckland, Auckland, New Zealand. DermNet Editor in Chief: Adjunct A/Prof Amanda Oakley, Dermatologist, Hamilton, New Zealand. Copy edited by Gus Mitchell/Maria McGivern. June 2019. DermNet Update July 2021
Introduction Other skin lesions with ABCDEFG features Melanomas without ABCDEFG features Importance What to do about concerning lesions
The 'ABCDE' of melanoma is an acronym designed to help the public and clinicians identify features in a skin lesion that may suggest an early or in situ melanoma (superficial spreading melanoma, lentigo maligna melanoma, or acral lentiginous melanoma).

Asymmetry of shape, structure and colour

Border irregularity

Colour variation
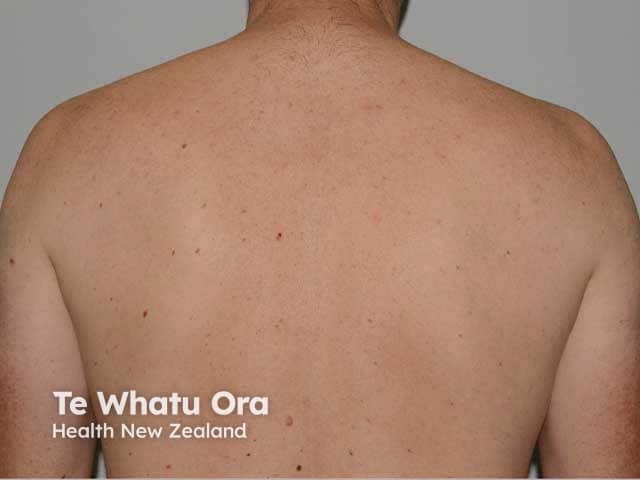
Different pigmented lesion just to the left of the spine between the shoulderblades
The EFG of melanoma is another acronym designed to help the public and clinicians identify skin changes in a lesion suggestive of nodular melanoma.
A is for Asymmetry.
A melanocytic naevus (harmless mole) is usually symmetrical, whereas melanoma is often irregular or asymmetrical in shape and/or colour.

Macro image of superficial spreading melanoma 8


0.8 mm lentigo maligna melanoma
B is for Border irregularity.
A melanocytic naevus has smooth, even borders, whereas a melanoma often has irregular, blurry, or jagged edges and hard-to-define border.
On careful inspection, the pigmented component of a flat melanocytic naevus fades out towards the edge, whereas the edges of a solar lentigo or a seborrhoeic keratosis are well defined. The edges of a melanoma tend to have both well-defined and fading segments.
B can also used for 'black', which is an uncommon colour for a melanocytic naevus in a white-skinned individual, but may be typical in skin of colour. The colour black however can occur in seborrhoeic keratoses in all skin types and ink spot lentigo in fair skin.

Melanocytic naevus with fading border

Seborrhoeic keratosis with sharp border

Melanoma with mixed sharp and fading border
C is for Colour variability.
A melanocytic naevus usually has a single shade of colour or two colours with one occurring inside the other or regularly repeated (generally pink, brown, or tan).

Pink dermal naevus

Melanocytic naevus

Dermal naevus
Melanoma can be brown (96%) but can have as many as five or six colours such as blue, black, tan, grey, pink, and red: 50% of melanomas include these uncommon colours. These colours are unevenly or irregularly distributed. C is also for Changing Colour.

Melanoma in situ

Invasive melanoma

Invasive melanoma
D is for Different.
Most people have a 'signature naevus' - all their melanocytic naevi resemble each other. A melanoma appears unique and very different from the patient’s other lesions.
A pigmented lesion that is obviously different from the others is sometimes called an 'ugly duckling', 'black sheep', 'lone ranger', or 'odd-mole-out' and must be considered suspicious even if it does not fulfil the ABCDEFG criteria.



E is for Evolving (changing).
A melanocytic naevus is usually stable and does not change in size, shape, or colour, whereas a melanoma changes over time. Change in size, colour, shape, or structure may be noted over months to years. However melanoma accounts for less than 3% of all changing skin lesions.

2012

2013

2017
E is for Elevated in the EFG acronym.
Benign lesions can be elevated (eg, a dermal naevus, dermatofibroma, or cyst), but a new elevated or thickened lesion may be suspicious for nodular melanoma or another form of skin cancer.
F is for Firm.
Benign lesions can feel firm (especially dermatofibroma), but this is also a feature of nodular melanoma.
G is for Growing
A nodular melanoma tends to grow rapidly with changes noted over days or weeks. Benign skin lesions tend to remain stable or change slowly over years to decades. Although they can rapidly change in appearance over hours to days if injured, inflamed, bleeding, or affected by eczema (eg, Meyerson naevus), they do not usually grow in size.

Nodular melanoma

Nodular melanoma

Nodular melanoma
The ABCDEFG criteria are not very specific for melanoma, as some or all of the criteria may be displayed by another skin cancer, such as a pigmented basal cell carcinoma or pigmented squamous cell carcinoma.

Pigmented basal cell carcinoma

Pigmented squamous cell carcinoma in situ

Pigmented actinic keratosis
A benign lesion can be asymmetrical in shape, have an irregular border, colour variation, and be different. Examples include congenital melanocytic naevus, atypical melanocytic naevus, solar lentigo, or seborrhoeic keratosis.
Melanocytic naevi can also evolve in some circumstances such as darkening after exposure to the sun, during pregnancy, and become more elevated with age; seborrhoeic keratoses and solar lentigines routinely evolve over time.
Clinicians trained in dermoscopy can often correctly diagnose skin lesions, but sometimes a biopsy will be needed to confirm a diagnosis.

Seborrhoeic keratosis

Solar lentigo

Melanocytic naevus
While the ABCDEFG criteria has been proven to be very helpful in identifying a potential melanoma, they cannot be used to reliably recognise all melanomas. A melanoma may be symmetrical in shape, with a uniform border, and without much colour variation.
The ABCDEFG criteria are particularly unhelpful in the diagnosis of some less common subtypes of melanomas such as desmoplastic melanoma and melanoma in childhood, as these often lack the ABCDEFG features.

Nodular melanoma

Amelanotic melanoma

Small melanoma
Melanoma is a serious form of skin cancer and can progress quickly. It is treatable if identified early but if it is untreated, it may spread to other parts of the body (metastatic melanoma) and this can be life-threatening.
Knowing the ABCDE and EFG features of melanoma can help you look for early signs of melanoma when performing a regular self-skin examination.
See our video on how to perform a self-skin examination.
If you have a skin lesion with ABCDE or EFG characteristics that concerns you, see your doctor as soon as possible for assessment. You may be referred to a specialist for another opinion and surgery.