What is basal cell naevus syndrome?
Basal cell naevus syndrome is a rare genetic cancer syndrome characterised by multiple early onset basal cell carcinomas, odontogenic keratocysts and other tumours, and other abnormalities.
Basal cell naevus syndrome (BCNS) is probably best known as Gorlin syndrome, and is also called naevoid basal cell carcinoma syndrome, amongst many other names.
Basal cell naevus syndrome
Who gets basal cell naevus syndrome?
Basal cell naevus syndrome is an autosomal dominant genetic disorder affecting males and females equally. Although seen in all races, race does influence incidence and penetrance with Gorlin syndrome rarely diagnosed in Black Americans and Asians. The prevalence is difficult to determine as although Gorlin syndrome has high penetrance, expressivity is variable and sporadic mutations are found in 50%. Estimates of prevalence range from 1/57,000 to 1/256,000.
What causes basal cell naevus syndrome?
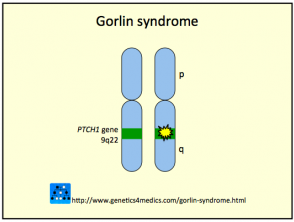
Basal cell naevus syndrome is the result of genetic mutations affecting the sonic hedgehog signalling pathway, a pathway crucial for proper cell differentiation. Genes implicated in Gorlin syndrome include PTCH1, PTCH2, and SUFU.
What are the clinical features of basal cell naevus syndrome?
Cutaneous features
- Multiple early onset cutaneous basal cell carcinomas (BCC)
- Usually present by 20 years of age
- Most common on sun-exposed sites, but can also occur on sun-protected sites such as the genitalia
- Smooth rounded papules, 1-15 mm in diameter
- May resemble skin tags, melanocytic naevi, haemangiomas, or milia
- Palmoplantar pits in up to 87%, often present in childhood
- Webbing of fingers and toes
- Milia and epidermoid cysts
Cutaneous features of basal cell naevus syndrome
Image Credit for palmar pits in skin of colour: Poladian K, Difato TC, Anderson KL, Taylor SL. Gorlin syndrome in a patient with skin type VI. Dermatol Online J. 2019;25(11):13030/qt64c4p1sq.
Skeletal features
- Characteristic facies — increased head circumference, hypertelorism, broad nasal root, fronto-parietal bossing, and enlarged mandible
- Skeletal abnormalities include bifid, splayed or fused ribs; kyphoscoliosis, wedge-shaped vertebrae; polydactyly, syndactyly; funnel chest (pectus excavatum) and pigeon chest (pectus carinatum)
Tumours
- Odontogenic keratocysts
- Multiple
- Usually located in the mandible
- Seen in up to 80%
- Present in the second and third decade
- Often asymptomatic but may cause pathological fracture and abnormal dentition
- Medulloblastoma — develops in childhood, found in 5%; only 3% of patients with medulloblastoma have BCNS
- 20x more common in those with a SUFU mutation
- Fibroma
- Cardiac fibroma — in 2% of children
- Ovarian fibromas — in 20% of females; bilateral; calcified
- Rhabdomyosarcoma
Ocular
- Corneal opacity, cataract, glaucoma, strabismus, retinal pigmentation, congenital blindness
Other
- Calcification of falx cerebri in 90% by age 20 years
- Gynaecomastia and hypogonadism in males
- Bicornuate uterus
- Cleft lip and palate, high arched palate
- Lymphatic cysts of the mesentery
- Intellectual impairment in up to 5%
How do clinical features vary in differing types of skin?
Basal cell carcinomas are seen in 80-90% of pale-skinned patients with Gorlin syndrome. Black patients may have < 2 skin cancers; 20% of dark-skinned Africans with Gorlin syndrome have none.
What are the complications of basal cell naevus syndrome?
- Aggressive invasive BCC on the eyelid or nose associated with local tissue destruction and high recurrence rate after treatment
- Metastatic cancer (rare)
- Psychosocial effects resulting from the many skin tumours and their treatment
How is basal cell naevus syndrome diagnosed?
Basal cell naevus syndrome can be diagnosed on clinical criteria alone but may require investigations to confirm it in some cases, particularly in children. The BCC histology is the same as for sporadic BCC [see Basal cell carcinoma pathology].
The diagnosis is made if there are two major criteria, or one major and two minor criteria.
Major criteria
- Five or more basal cell carcinomas in a lifetime, or BCC before age 20 years, or excessive numbers out of proportion to prior sun exposure or skin type
- Histologically proven odontogenic keratocyst
- Palmar and/or plantar pits (3 or more)
- Lamellar calcification or obvious calcification of the falx cerebri before the age of 20 years
- Bifid, fused, or splayed ribs
- First degree relative with basal cell naevus syndrome
- PTCH1 mutation
Minor criteria
- Medulloblastoma
- Macrocephaly with occipitofrontal circumference > 97th percentile
- Congenital malformations, including lymphomesenteric or pleural cysts, cleft lip or palate
- Skeletal abnormalities
- Cardiac or ovarian fibroma
What is the differential diagnosis for basal cell naevus syndrome?
- Chronic sun exposure
- Xeroderma pigmentosum
- Other genodermatoses with multiple BCC —including Bazex-Dupré-Christol syndrome, Rombo syndrome
What is the treatment for basal cell naevus syndrome?
General measures and screening
- Genetic counselling
- Multidisciplinary care
- Sun protection
- Brain MRI screening every 6 months for medulloblastoma to age 3 years, then annual for age 3–8 years
- Cardiac ultrasound for cardiac fibromas in children
- Annual X-rays for dental cysts
- Abdominal and pelvic ultrasound starting at puberty for ovarian fibromas and mesenteric cysts
- Regular complete skin examination every 2–3 months for adults, and self skin examination
- Neurological, ophthalmological, cardiac, orthopaedic, and urogynaecological examinations
- Radiotherapy is contraindicated due to the increased risk of skin cancer
Specific measures
- Medulloblastoma — surgery and chemotherapy
- Basal cell carcinomas — options include:
- Small superficial BCC in non-critical sites — curettage & cautery, cryotherapy, 5-fluorouracil, imiquimod, photodynamic therapy,
- Large or aggressive BCC — excision; consider Mohs surgery
- Multiple BCC — electrochemotherapy with bleomycin under sedation
- Hedgehog inhibitors such as vismodegib (oral) and sonidegib (topical).
- Odontogenic keratocysts — peripheral osteotomy with curettage
What is the outcome for basal cell naevus syndrome?
Basal cell naevus syndrome patients continue to develop new BCC throughout their life, with some patients having over 1000 BCC in their lifetime (median 8). Basal cell carcinomas can be clinically aggressive causing considerable morbidity and can be fatal. Life expectancy is generally believed to not otherwise be affected.