Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Author: A/Prof Amanda Oakley, Dermatologist, Hamilton, New Zealand, February 2016.
Introduction Introduction - hirsuitism Introduction - hypertrichosis Demographics for hirsutism Demographics for hypertrichosis Causes Causes of hypertrichosis Clinical features Complications Diagnosis Treatment Prevention Outlook
Excessive hair comprises two entities:
Hirsutism is a male pattern of secondary or post-pubertal hair growth occurring in women. It arises in the moustache and beard areas at puberty when hair also appears in non-hirsute women in the underarm and pubic regions. Hirsute women may also develop thicker, longer hair than is usual on their limbs and trunk.
Hirsutism is also known as hirsutes.

Facial hirsutism

Facial hirsutism

Facial hirsutism
Hypertrichosis is non-hirsute excessive hair growth over and above the normal for the age, sex and race of a male or female. It can refer to unpigmented vellus hair or darker, longer, terminal hair, and can be generalised or localised.

Hypertrichosis

Hypertrichosis

Hypertrichosis
Which women are considered hirsute varies according to culture and ethnicity, as the normal range of secondary hair growth varies with race. It should also be noted that women spend a great deal of time and energy removing unwanted hair, resulting in an unnaturally hair-free norm in today’s society.
Hyperandrogenism is often associated with polycystic ovaries, insulin resistance and obesity. Rare causes include:
Hair growth is genetically determined and highly variable. Hypertrichosis may be a subjective complaint of healthy individuals. Pathological hypertrichosis can be congenital or acquired.
Generalised acquired hypertrichosis may be associated with:
Localised acquired hypertrichosis may be associated with:
Different genes expressed in individual hair follicles vary in their response to androgens.
Hypertrichosis is due to non-hormonal alteration in hair growth driven by genes and cytokines. Precise causes in an individual are often unknown.
Hirsutism is usually first noted in late teenage years and tends to get more severe as the woman gets older. Hypertrichosis can be present at birth or appear at any time later on. Affected areas vary.
Hirsutism is usually isolated. It can involve a single site or multiple sites.
The severity of hirsutism is assessed using a modified version of the Ferriman-Gallwey visual scale for nine areas of the body. The score varies from 0 (no hair) to 4 (extensive hair growth) in each area.
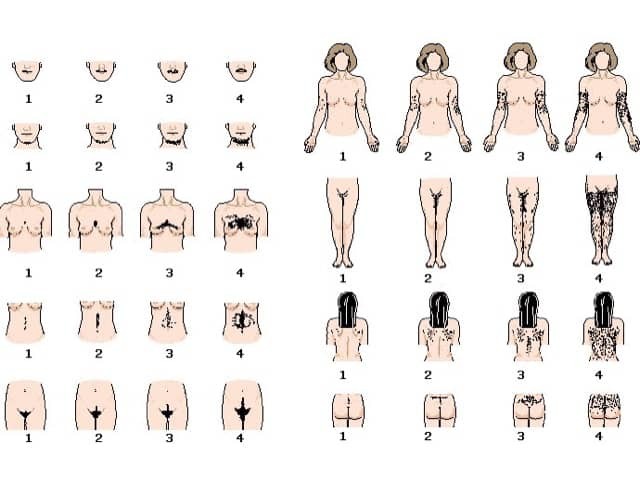
Ferriman-Gallwey visual scale for assessing hirsutism
A general examination may reveal clues as to the cause of hirsutism.
People affected by excessive hair may suffer from great embarrassment with psychosocial effects. They may go to considerable lengths and expense to remove the hair.
Other complications can arise from underlying disease if any.
Hirsutism and hypertrichosis are diagnosed clinically. Investigations are not usually necessary unless the Ferriman-Gallwey score is > 15 when blood tests are done to evaluate male hormone levels and underlying diseases.
Free androgen index is total testosterone concentration divided by sex hormone binding globulin concentration and multiplied by 100. If elevated, check:
If early-onset of hirsutism, premature adrenarche, and family history of congenital adrenal hyperplasia:
If Cushingoid features:
If menstrual disorder:
If symptoms suggest poor general health:
If suspicious of polycystic ovaries:
Diagnostic features for polycystic ovary syndrome are:
If there is skin fragility or blisters in sun-exposed sites:
If there is a faun tail:
Bleaching makes the excessive hair less obvious.
Hair removal (epilation and depilation) needs to be regularly repeated as the hair continues to grow back. Methods include:
Hair removal creams containing eflornithine are available on prescription in some countries.
Some women with hirsutism may be treated with antiandrogens with variable response. This option is not useful in hypertrichosis. Drugs to consider include:
It is not yet possible to prevent genetically predetermined excessive hair growth. Insulin resistance associated with obesity can be reduced by weight loss and dietary control.
Prognosis depends on the cause. The most common types of excessive hair growth persist life-long. Hirsutism tends to be more pronounced with age.