What is pemphigus vulgaris?
Pemphigus vulgaris is a rare autoimmune disease that is characterised by painful blisters and erosions on the skin and mucous membranes, most commonly inside the mouth. Pemphigus vulgaris accounts for 70% of all pemphigus cases worldwide although it is extremely rare in New Zealand (about one case per million of the population).
The other main subtypes of pemphigus are:
- Pemphigus foliaceus and allied disorders
- Pemphigus erythematosus (an overlap of pemphigus foliaceus and lupus erythematosus)
- Pemphigus herpetiformis
- Pemphigus vulgaris and allied disorders
- IgA pemphigus
- Pemphigus vegetans
- Paraneoplastic pemphigus.
Pemphigus vulgaris
See more pemphigus vulgaris images
Who gets pemphigus vulgaris?
Pemphigus vulgaris affects people of all races, age, and sex. It most commonly appears between the ages of 30 and 60 years and is more common in Jews and Indians than in other races, presumably for genetic reasons.
Drug-induced pemphigus is also recognised and is most often caused by penicillamine, angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, and cephalosporins.
Pemphigus is sometimes triggered by cancers particularly lymphomas and Castelman disease (paraneoplastic pemphigus), infection, or trauma.
What causes pemphigus vulgaris?
Pemphigus vulgaris is an autoimmune blistering disease.
The keratinocytes are cemented together at unique sticky spots called desmosomes. In pemphigus vulgaris, immunoglobulin type G (IgG) autoantibodies bind to a protein called desmoglein 3 (dsg3), which is found in desmosomes in the keratinocytes near the bottom of the epidermis. The result is the keratinocytes separate from each other, and are replaced by fluid (the blister). About 50% of patients with pemphigus vulgaris also have anti-dsg1 antibodies.
What are the clinical features of pemphigus vulgaris?
Most patients with pemphigus vulgaris first present with lesions on the mucous membranes such as the mouth and genitals. Blisters usually develop on the skin after a few weeks or months, although in some cases, mucosal lesions may be the only manifestation of the disease.
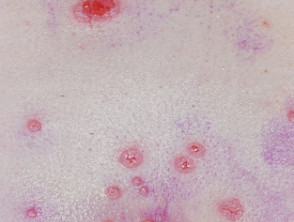
Skin lesions appear as thin-walled flaccid blisters filled with clear fluid that easily rupture causing itchy and painful erosions. They most often arise on the upper chest, back, scalp, and face. Erosions in the skin folds may develop into vegetative lesions which are granular and crusted (pemphigus vegetans). The skin around the nails may be painful, red, and swollen.
Cutaneous pemphigus vulgaris
In comparison to white skin, darker skin tones may differ in their presentation which can cause diagnostic delay. Diagnostic features in darker skin tones may include flaccid blister which lack erythema and hyperpigmented plaques with superficial erosion and haemorrhagic crusting. At later and more advanced stages, plaques with a pink base and surrounding hyperpigmentation are present.
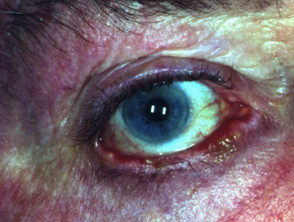
The inside of the mouth is commonly involved in pemphigus vulgaris. Involvement of the pharynx and larynx cause pain on swallowing and a hoarse voice. Nasal involvement causes congestion and bleeding. The conjunctiva, oesophagus, labia, vagina, cervix, penis, urethra and anus may also be affected.
Features of oral mucosal pemphigus include:
- Oral lesions in 50–70% of patients
- Superficial blistering and erosions
- Widespread involvement within the mouth
- Painful, slow-to-heal ulcers
- Spread to the larynx causing hoarseness when talking
- Difficulty eating and drinking.
Mucosal pemphigus vulgaris
See more pemphigus vulgaris images
Clinical variants of pemphigus vulgaris
Pemphigus vegetans
- Rare subtype, characterised by vegetative plaques composed of excessive granulating tissue and crusting.
- Accounts for 1-2% cases of all pemphigus and most commonly occurs at intertriginous sites, face and scalp.
- Characteristic histological finding include hyperkeratosis, pseudoepitheliomatous hyperplasia and papillomatosis with acantholysis that creates a suprabasal cleft.
- Two clinical subtypes:
- pemphigus vegetans of Neumann (vegetative plaques arising from pemphigus vulgaris lesions)
- Pemphigus vegetans of Hallopeau (plaques not preceded by bullae).
Pemphigus herpetiformis
- Previously described a rare subtype of pemphigus vulgaris or pemphigus foliceus.
- Characterised by urticarial plaques and vesiculobullous eruption seen in herpetiform or annular pattern.
- Plaques are associated with severe pruritus and rarely involve the mucosa.
- Histologically characterised by eosinophilic spongiosis, mostly without acantholysis.
What are the complications of pemphigus vulgaris?
Pemphigus vulgaris can cause very extensive, life-threatening erosions, especially if the diagnosis is delayed. Other potentially severe complications may include:
- Secondary bacterial infection
- Fungal infection, especially candida
- Viral infection, especially herpes simplex
- Nutritional deficiencies due to difficulty eating
- Complications of systemic steroids especially infections and osteoporosis
- Complications of immune suppressive treatments
- The psychological effects of severe skin disease and its treatment (anxiety and depression).
How is pemphigus vulgaris diagnosed?
Diagnosis of pemphigus vulgaris generally requires a biopsy of a blister. Diagnosis of pemphigus vulgaris generally requires a biopsy from the skin adjacent to a lesion. Histology typically shows rounded-up and separated keratinocytes (acantholytic cells) just above the basal layer of the epidermis. Suprabasal clefting may be reported. See pathology of pemphigus vulgaris.
Pemphigus is confirmed by direct immunofluorescence staining of perilesional skin biopsy sections to reveal immunoglobulin (Ig)G antibodies or complement on the cell surfaces of keratinocytes.
In most cases, circulating antibodies can be detected by a blood test (indirect immunofluorescence test). The level of antibodies fluctuates and may reflect the effectiveness of treatment. Specific anti-dsg1 and anti-dsg3 antibody titres can also be measured in blood or saliva by enzyme-linked immunosorbent assays (ELISAs).
Pemphigus vulgaris may co-exist with or be confused with pemphigus foliaceus, cicatricial pemphigoid and lichen planus.
How is the severity of pemphigus vulgaris assessed?
The severity of pemphigus can be scored using various scoring systems.
- PDAI: Pemphigus Disease Area Index
- PAAS: Pemphigus Area and Activity Score
- PAS: Pemphigus Activity Score
- ABSDIS: Autoimmune Bullous Skin Disorder Intensity Score
- Saraswat oral pemphigus scoring
- Pemphigus vulgaris lesion severity score
- Harman pemphigus grading
- Kumar scoring system
- Mahajan scoring system
What is the treatment of pemphigus vulgaris?
The primary aim of treatment of pemphigus vulgaris is to decrease blister formation, prevent infections and promote healing of blisters and erosions [4.5]. Systemic corticosteroids >are the mainstay of medical treatment for controlling the disease, usually in the form of moderate to high doses of oral prednisone or prednisolone, or as pulsed intravenous methylprednisolone. Since their use, many deaths from pemphigus vulgaris have been prevented (the mortality rate dropped from 99% to 5–15%). Corticosteroids are not a cure for the disease but improve the patient's quality of life by reducing disease activity. The doses of corticosteroids needed to control pemphigus vulgaris and the length of time on treatment may result in serious side effects and risks.
Other immunosuppressive drugs (mostly off-label) used to reduce the dose of steroids and may be required by patients with pemphigus vulgaris for years. These are most often:
- Azathioprine
- Mycophenolate mofetil
- Cyclophosphamide
- Rituximab, which is now approved by the Food and Drug Administration (FDA) in the US.
Other medications that are sometimes used in pemphigus (often in combination) include:
- Dapsone
- Methotrexate
- Tetracyclines
- Nicotinamide
- Plasmapheresis
- Intravenous immunoglobulin
- Extracorporeal photopheresis
- Immunoadsorption
- The TNFα inhibitor, infliximab.
At optimal therapy, patients may continue to experience mild disease activity.
Other considerations include vaccination (live vaccines are contraindicated), bone prophylaxis, baseline ophthalmological assessment, and psychological support if needed.
Topical therapy
Topical therapy for cutaneous pemphigus vulgaris may include topical steroids and emollients.
Treatment of mucosal pemphigus vulgaris may include various formulations of a topical steroid, intralesional steroid, topical tacrolimus, or topical ciclosporin.
General management
Appropriate wound care is particularly important, as this should promote healing of blisters and erosions.
- Handle skin very gently to avoid causing new blisters and erosions.
- Wear surgical gloves and use aseptic technique when changing dressings.
- Analgesics may be needed especially for dressing changes.
- Gently cleanse with an antiseptic solution or take a bleach bath.
- Drain intact blisters, but leave the blister roof in place.
- Apply a bland emollient ointment, such as 50% white soft paraffin + 50% liquid paraffin, directly to the skin, or apply the ointment to a dressing.
- Use non-adherent dressings (such as petrolatum-soaked gauze or silicone mesh). These may incorporate an antiseptic.
- An absorbent dressing may be applied over the primary dressing if the erosions are oozing.
- Be vigilant in identifying and treating any infection.
Patients should minimise activities that may traumatise the skin and mucous membranes during active phases of the disease. These include activities such as contact sports and eating or drinking food that may irritate or damage the inside of the mouth (spicy, acidic, hard and crunchy foods).
Oral hygiene and proper dental care are essential.
- Use a soft toothbrush and mint-free toothpaste to gently and thoroughly brush teeth twice daily.
- Rinse using an antiseptic or anti-inflammatory mouthwash.
- Treat oral candidiasis, if present.
Future prospects for treatment
There is future hope that future treatment for pemphigus will be more specific with fewer side effects. The CD20 antagonist ofatumumab has been reported to be effective. Investigators have engineered specific chimeric autoantibody receptor T-cells to eliminate desmoglein-3-specific B cells in mice. The use of anti-neonatal Fc receptor is under investigation in combination with rituximab.