Main menu
Common skin conditions

NEWS
Join DermNet PRO
Read more
Quick links
Author: Dr Amanda Oakley, Dermatologist, Hamilton, New Zealand, 1996. Updated by Dr Jannet Gomez, Postgraduate student in Clinical Dermatology, Queen Mary University London, UK, December 2016. Updated February 2021 and minor update November 2025.
Introduction
Demographics
Causes
Clinical features
Complications
Diagnosis
Differential diagnoses
Treatment
Outcome
A viral wart is a very common benign lesion caused by infection with human papillomavirus (HPV). Viral warts can be classified by site as being cutaneous or mucosal as the HPV types are quite distinct [see Anogenital wart and Sexually acquired human papillomavirus for further information on mucosal HPV infection]. A cutaneous wart is also called a verruca or papilloma, and warty-looking lesions of any cause may be described as verrucous or papillomatous.

Common warts

Plane warts

Filliform wart
See more images of viral warts.
Warts are particularly common in:
Warts are due to infection by the human papillomavirus (HPV), a double-stranded DNA virus. There are more than 150 known HPV types, only some of which infect the skin, giving rise to a variety of clinical presentations. Infection begins in the basal layer of the epidermis, causing proliferation of the keratinocytes (skin cells) and hyperkeratosis, and production of infectious virus particles — the wart. The most common HPV types infecting the skin are types 1, 2, 3, 4, 10, 27, 29, and 57.
HPV is spread by direct skin-to-skin contact or autoinoculation; if a wart is scratched or picked, a wart may develop under the fingernail (subungual wart) or virus may be spread to another area of skin. Autoinoculation of the virus in a scratch can result in a line of warts (pseudo-koebnerisation) The incubation period can be as long as twelve months, depending on the amount of virus inoculated.
[see Non-sexually acquired human papillomavirus infection]

Pseudo-koebnerisation of warts

Subungual wart

Subungual wart
Cutaneous viral warts have a hard, keratinous surface. Tiny red or black dots visible in the wart are papillary capillaries.
Common warts (verruca vulgaris) present as cauliflower-like papules with a rough, papillomatous and hyperkeratotic surface ranging in size from 1 mm to 1 cm or more. They may be solitary or multiple. Common warts are found most often on the knees, backs of fingers or toes, and around the nails (periungual).


Verruca vulgaris on a thumb

Plantar warts (verruca plantaris) include tender inwardly growing myrmecia on the sole caused by HPV 1, and clusters of superficial less painful mosaic warts due to HPV 2. Myrmecial warts are typically tender with lateral and direct pressure, are surrounded by yellow hyperkeratotic callus-like skin showing accentuated skin markings, but with discontinuation of the skin lines through the actual wart.
Plantar epidermoid cysts are associated with HPV 60 infection of the eccrine ducts.



Plantar warts



Plane warts are typically multiple small flat-topped skin-coloured papules located most commonly on the face, hands, and shins. On the shins and beard-area of the face the virus is often spread by shaving resulting in numerous warts. Plane warts are mostly caused by HPV types 3 and 10.


Verruca plana in the beard area spread by shaving

A filiform wart is a cluster of fine fronds emerging from a narrow pedicle base usually found on the face. They are also described as digitate (finger-like).



Filiform wart
Butcher's warts are specifically caused by HPV 7 infecting the hands of butchers and others whose occupation involves chronic exposure to a cold moist environment. They clinically resemble common warts and tend to be numerous.
Epidermodysplasia verruciformis is a rare autosomal recessive condition susceptible to skin infection with specific HPV types that cause flat pityriasis versicolor-like lesions and squamous cell carcinoma.


Ungual wart

Cutaneous viral warts are usually diagnosed clinically. Clinical clues to diagnosis can include:
Dermoscopy assists visualisation of the papillary capillaries of a viral wart, and can distinguish other verrucous lesions such as a seborrhoeic keratosis.

Red and black pinpoint dots of papillary capillaries
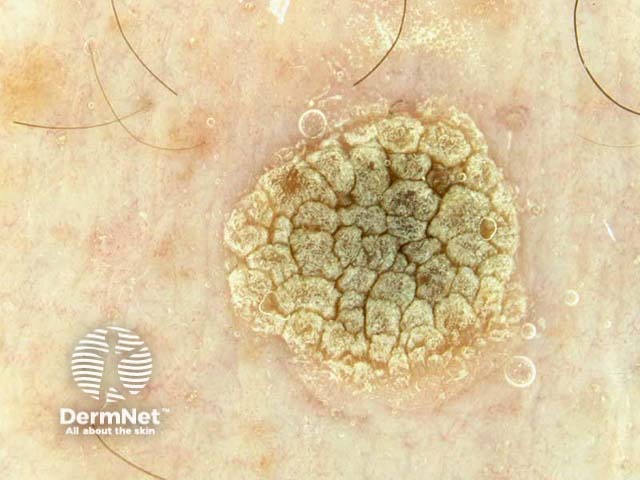
Dermoscopy: viral wart
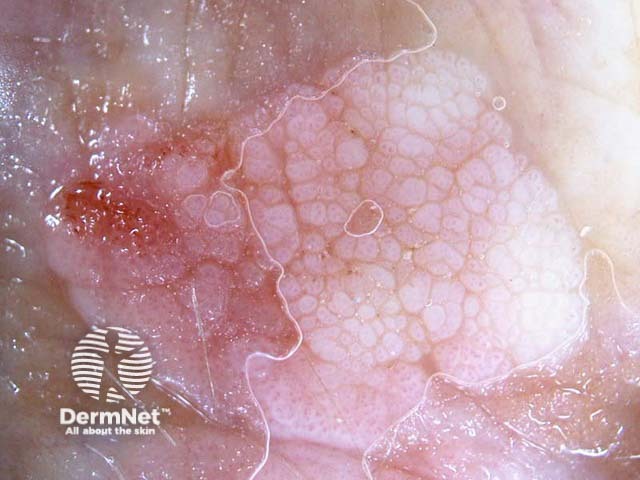
Dermoscopy: viral wart
Skin biopsy is sometimes required when squamous cell carcinoma cannot be excluded clinically such as in an organ transplant recipient susceptible to both. [see Verruca vulgaris pathology, Verruca plana pathology]
Differential diagnoses for a cutaneous viral wart can include:
Treatment may not be required in all cases as most warts resolve spontaneously especially in children. Indications for active treatment include:
Treatments do not kill the virus, but work by removing virus-containing skin. Persistence with the treatment and patience is essential! Remember HPV infects the basal cell layer of the epidermis so warts recur rapidly if the virus has not been eradicated.
Topical treatment includes wart paints, pastes, or patches containing salicylic acid, podophyllin, or similar compounds, which work by removing the surface skin cells.
Topical treatment is applied once daily to the wart. Treatment with wart paint usually makes the wart smaller and less uncomfortable; 70% of warts resolve within twelve weeks of daily applications.
If the wart paint makes the skin sore, stop treatment until the discomfort has settled, then recommence as above.
Cryotherapy with liquid nitrogen is repeated at one to two–week intervals to cause peeling of the surface layer. It is uncomfortable and results in blistering for several days or weeks. Treatment is required frequently to prevent the wart regrowing between appointments. Success is in the order of 70% after 3–4 months of regular freezing.
A hard freeze using liquid nitrogen might leave a permanent white mark. It can also cause temporary numbness if performed over a superficial nerve such as on the side of a finger.

Cryotherapy for warts
Electrosurgery (curettage and cautery) has been used for large and resistant warts. Under local anaesthetic, the growth is pared away and the base burned. The wound heals in two weeks or longer (depending on the site); even then 20% of warts can be expected to recur within a few months. This treatment leaves a permanent scar which can be painful to walk on if located on a pressure site. Recurrent wart in a scar is very hard to treat.
Other treatments for recurrent, resistant or extensive warts include:
Vaccines against human papillomavirus are available to prevent anogenital warts. Anecdotally, these have been reported to result in the clearance of non-genital warts in some people without definite evidence that the vaccine is the cause of remission.
No treatment is universally effective at eradicating viral warts.
In children, even without treatment, 50% of warts disappear within six months, and 90% are gone in 2 years.
Viral warts are more persistent in adults, but they clear up eventually. They are likely to recur in patients that are immunosuppressed, for example, organ transplant recipients. Recurrence is more frequent in tobacco smokers.
Immunity to HPV is likely to be type-specific.