What is a cyst?
A cyst is a benign, round, dome-shaped encapsulated lesion that contains fluid or semi-fluid material. It may be firm or fluctuant and often distends the overlying skin. There are several types of cyst. The most common are described here.
What is a pseudocyst?
Cysts that are not surrounded by a capsule are better known as pseudocysts. These commonly arise in acne.
Who gets cysts?
Cysts are very common, affecting at least 20% of adults. They may be present at birth or appear later in life. They arise in all races. Most types of cyst are more common in males than in females.
What causes cysts?
The cause of many cysts is unknown.
- Epidermoid cysts are due to the proliferation of epidermal cells within the dermis. Their origin is the follicular infundibulum. Multiple epidermoid cysts may indicate Gardner syndrome. The common term, sebaceous cyst, is a misnomer.
- An epidermal inclusion cyst is a response to an injury. Skin is tucked in to form a sac that is lined by healthy epidermal cells that continue to multiply, mature and form keratin.
- The origin of a trichilemmal cyst is hair root sheath. Inheritance is autosomal dominant (the affected gene is within the short arm of chromosome 3) or sporadic.
- The origin of steatocystoma is the sebaceous duct within the hair follicle. Steatocystoma multiplex is sometimes an autosomal dominantly inherited disorder due to mutations localised to the keratin 17 (K17) gene, when it may be associated with pachyonychia congenita. More often, steatocysts are sporadic, when these mutations are not present.
- The origin of the eruptive vellus hair cyst is follicular infundibulum. It may be inherited as an autosomal dominant disorder due to mutations in the keratin gene.
- A dermoid cyst is a hamartoma, a developmental error.
- The origin of a ganglion cyst is degeneration of the mucoid connective tissue of a joint.
- Occlusion of pilosebaceous units (hair follicles) or eccrine sweat ducts leads to a build-up of secretions, which can present as milia.
- Occlusion of the orifice of a mucous gland can lead to a fluid-filled mucocoele in a mucous membrane (lip, vulva, vagina).
- A milium is a pseudocyst due to failure to release keratin from an adnexal structure. The origin of primary milium is infundibulum of the vellus hair follicle at the level of the sebaceous gland and is a miniature version of an epidermoid cyst. The source of secondary milium is a retention cyst within a vellus hair follicle, sebaceous duct, sweat duct or epidermis.
- Pseudocysts in acne are formed by occlusion of the follicle by keratin and sebum.
What are the clinical features of cysts?
Epidermoid cyst
- Epidermoid cysts occur on face, neck, trunk or anywhere where there is little hair.
- Most epidermoid cysts arise in adult life.
- They are more than twice as common in men as in women.
- They present as one or more flesh–coloured to yellowish, adherent, firm, round nodules of variable size.
- A central pore or punctum may be present.
- Keratinous contents are soft, cheese-like and malodorous.
- Scrotal and vulval cysts are frequently multiple and may calcify.
An epidermoid cyst is also called a follicular infundibular cyst, epidermal cyst, and keratin cyst.
Epidermoid cyst
See more images of epidermoid cysts.
Trichilemmal cyst
- 90% of trichilemmal cysts occur on the scalp; otherwise face, neck, trunk, and extremities.
- Most trichilemmal cysts arise in middle age.
- In 70% of cases, trichilemmal cysts are multiple.
- They present as adherent, round or oval, firm nodules.
- There is no punctum.
- The keratinous content is firm, white and easily enucleated.
A trichilemmal cyst is also called pilar cyst.
Trichilemmal cyst
See more images of epidermoid cysts.
Steatocystoma
- A solitary steatocystoma is known as steatocystoma simplex.
- More often, there are multiple lesions (steatocystoma multiplex) on the chest, upper arms, axillae, neck and scrotum or vulva.
- The cysts arise in the late teens and 20s due to the effect of androgens and persist lifelong.
- They are freely moveable, smooth flesh to yellow colour papules 3–30 mm in diameter.
- There is no central punctum.
- Content of cyst is predominantly sebum.
Steatocystoma multiplex
Eruptive vellus hair cysts
- Eruptive vellus hair cysts are present in childhood if familial, and later if sporadic.
- They are seen in association with steatocystoma multiplex.
- Multiple 2–3 mm papules develop over the sternum.
- The cysts contain vellus hairs.
Dermoid cyst
- A cutaneous dermoid cyst may include skin, skin structures and sometimes teeth, cartilage and bone.
- Most dermoid cysts are found on face, neck, scalp; often around eyelid, forehead and brow.
- It is a thin-walled tumour that ranges from soft to hard in consistency.
- The cyst is formed at birth, but the patient may not present until an adult.
Dermoid cysts
Ganglion cyst
- A ganglion cyst most often involves the scapholunate joint of the dorsal wrist.
- These arise in young to middle-aged adults.
- They are three times more common in women than in men.
- The cyst is a unilocular or multilocular firm swelling 2–4 cm in diameter that transilluminates.
- Cyst contents are mainly hyaluronic acid, a golden-coloured goo.
Ganglion cyst
Digital myxoid pseudocyst
- Mucous/myxoid pseudocysts arise in older adults on the distal phalanx
- They arise from distal interphalangeal joint, associated with osteoarthritis.
- They often present as a longitudinal depression in the nail due to compression on the proximal matrix.
Myxoid pseudocyst
See more images of digital myxoid pseudocysts.
Labial mucous/myxoid cyst
- A cyst in the lip may be due to occlusion of the salivary duct
- A labial cyst is also called a mucocoele.
- It is a soft to firm, 5–15 mm diameter, semi-translucent nodule.
Mucocoele of lip
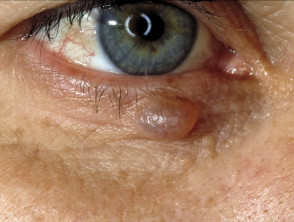
Hidrocystoma
- Hidrocystoma is a translucent jelly-like cyst arising on an eyelid.
- It is also known as cystadenoma, Moll gland cyst, and sudoriferous cyst.
- The common solitary translucent eyelid cyst is an apocrine hidrocystoma.
- Multiple cysts on the lower eyelid are eccrine hidrocystomas.
- Link to apocrine hidrocystoma – pathology.
Hidrocystoma of eyelid
More images of hidrocystoma of the eyelid.
Milium/milia
- Milia are 1–2 mm superficial white dome-shaped papules containing keratin
- Primary milia arise in neonates (50%), adolescents and adults; they are rarely familial and sometimes eruptive.
- Primary milia occur on eyelids, cheeks, nose, mucosa (Epstein pearls) and palate (Bohn nodules) in babies; and eyelids, cheeks and nose of older children and adults.
- Transverse primary milia are sometimes noted across the nasal groove or around the areola.
- In milia en plaque, multiple milia arise on an erythematous plaque on face, chin or ears.
- Secondary milia arise at the site of epidermal repair after blistering or injury, in epidermolysis bullosa, bullous pemphigoid, porphyria cutanea tarda, thermal burn, and after dermabrasion.
- Secondary milia are reported as an adverse effect of topical steroids, 5-fluorouracil cream, vemurafenib and dovitinib.
Milia
Vulval mucous cyst
- A vulval mucous cyst is due to occlusion of Bartholin or Skene duct.
- It presents as a soft swelling in the introitus of the vagina: a posterior swelling is a Bartholin cyst and a periurethral swelling is a Skene cyst.
Comedo and acne pseudocyst
- Comedones are pseudocysts formed by occlusion of the follicle by keratin and sebum.
- The open comedo (blackhead) and closed comedo (whitehead) are small, superficial papules typical of acne vulgaris
- Solar comedones arise in sun-damaged skin and are associated with smoking.
- Large uninflamed pseudocysts accompany inflammatory nodules in nodulocystic acne and hidradenitis suppurativa.
Comedones
Pseudocyst of auricle
- Pseudocyst of the auricle (external ear) follows trauma.
Pseudocyst of auricle
Complications of cysts
Rupture of a cyst
- The contents of the cyst may penetrate the capsular wall and irritate the surrounding skin.
- The area of tender, firm inflammation spreads beyond the encapsulated cyst.
- Sterile pus may be discharged.
Secondary infection
- A ruptured cyst may infrequently become secondarily infected by Staphylococcus aureus, forming a furuncle (boil).
Pressure effect
- A dermoid cyst can cause pressure on underlying bony tissue.
- A ganglion cyst can cause joint instability, weakness, limitation of motion and may compress a nerve.
- A digital mucous cyst may place pressure on the proximal matrix and cause a malformation of the nail.
Malignancy
- Cutaneous cysts and pseudocysts are non-proliferative benign lesions.
- Nodulocystic basal cell carcinoma is a common skin cancer that presents as a rounded nodule and may initially be mistaken for a cyst, but steady enlargement, destruction of the epidermis with ulceration and bleeding occur eventually.
- A malignant proliferative trichilemmal cyst is a misnomer. It is an extremely rare tumour.
How are cysts diagnosed?
Cysts have typical clinical characteristics. When a cyst is surgically removed, it should undergo a histological examination. The type of lining of the wall of the cyst and the cyst contents help the pathologist classify it.
- An epidermoid cyst is lined with stratified squamous epithelium that contains a granular layer. Laminated keratin contents are noted inside the cyst. An inflammatory response may be present in cysts that have ruptured.
- Trichilemmal cysts have a palisaded outer layer without a granular layer. The contents are eosinophilic hair keratin. Older cysts may exhibit calcification. The proliferating variety is considered a tumour.
- Steatocystoma has a folded cyst wall with prominent sebaceous gland lobules.
- A dermoid cyst contains fully mature elements of the skin including fat, hairs, sebaceous glands, eccrine glands, and in 20%, apocrine glands.
- The lining of the wall of a ganglion cyst or digital mucous cyst is collagen and fibrocytes. It contains hyaline material.
- Hidrocystoma has a thin lining wall of eosinophilic bilaminar cells.
What is the treatment for cysts?
An asymptomatic epidermoid cyst does not need to be treated. In most cases, an attempt to remove only the contents of a cyst is followed by recurrence. If desired, cysts may be entirely excised. Recurrence is not uncommon, and re-excision may be surgically challenging.
Inflamed cysts are sometimes treated with:
- Incision and drainage
- Intralesional injection with triamcinolone
- Oral antibiotics
- Delayed excision biopsy
How can cysts be prevented?
Unknown.
What is the outlook for cysts?
Cysts generally persist unless surgically removed.