What is sarcoidosis?
Sarcoidosis is a multisystem disease characterised by granulomas in various organs. Characteristically, these are non-caseating epithelioid granulomas (a pathological description distinguishing sarcoidal granulomas from the caseating or cheese-like granulomas seen in tuberculosis).
Sarcoidosis can affect a variety of organs with varying frequencies, including:
- Lungs
- Skin
- Eye
- Liver
- Heart
- Nervous system
- Musculoskeletal.
Sarcoidosis
Who is at risk of sarcoidosis?
Sarcoidosis occurs worldwide, affecting persons of all races, ages, and sex.
- African Americans and Scandinavians have a higher incidence of the disease.
- Sarcoidosis mainly affects people between 30-50 years of age.
- It is more prevalent in women, non-smokers, and rural communities.
- Its incidence is estimated to be between 2.3 and 11 per 100,000 individuals/year.
What causes sarcoidosis?
No single cause has been identified. Many researchers have hypothesized the role of genetics, environmental factors, and autoimmunity in the development of sarcoidosis.
Genetics
Eleven sarcoidosis genetic risk loci (BTNL2, HLA-B, HLA-DPB1, ANXA11, IL23R, SH2B3/ATXN2, IL12B, NFKB1/MANBA, FAM177B, chromosome 11q13.1, and RAB23) have been identified.
Several HLA and non-HLA alleles are associated with the development of this disease such as HLA-DRB1*0301/ DQB1*0201, transforming growth factor β (TGF-β), tumour necrosis factor α (TNF-α), and Toll-like receptor 4 (TLR-4). Monozygotic twins with sarcoidosis have an 80-fold higher risk of also developing sarcoidosis.
Environmental factors and autoimmunity
Exposure to substances such as wood stoves, soil, tree pollen, inorganic particulates, insecticides, and silica have been associated with an increased risk of developing sarcoidosis.
It has been suggested that certain bacteria may trigger sarcoidosis including Mycoplasma species, Leptospira species, herpes virus, retrovirus, Chlamydia pneumoniae, Borrelia burgdorferi, Pneumocystis jirovecii, and Propionibacterium species.
Drug-induced sarcoidosis-like reactions have been reported with a number of medications, including checkpoint inhibitors, and anti-TNF and anti-interleukin biological agents.
What are the signs and symptoms of sarcoidosis?
Sarcoidosis can affect any organ therefore patients may present with a wide variety of symptoms.
Sarcoidosis may not result in any symptoms and the disease may come and go without the patient or doctor ever being aware of it. Symptoms can appear suddenly and then just as quickly resolve spontaneously. Sometimes, however, they can continue over a lifetime.
Non-specific general symptoms like fatigue are seen in nearly 70% of patients. Other constitutional symptoms may include:
- Weight loss
- Loss of appetite
- Fever
- Chills and night sweats.
More than 20% of patients have peripheral lymphadenopathy. The affected lymph nodes are moderately swollen and are usually painless.
Sarcoidosis may involve one organ system or several.
Symptoms and signs of specific organ involvement
Lungs
- Respiratory symptoms are found on presentation in 30-53%.
- These include coughing, shortness of breath, and chest pain. Almost half of patients with pulmonary sarcoidosis may be asymptomatic.
- In some patients, upper respiratory tract involvement produces hoarseness, nasal obstruction, and recurrent or persistent sinusitis.
- Bilateral perihilar lymphadenopathy and pulmonary nodules may be seen on chest x-ray and CT thorax. Pulmonary fibrotic changes may also be seen.
Skin (cutaneous sarcoidosis) and mucosae
- Skin involvement is present in up to one-third of patients.
- About 30% of patients with cutaneous sarcoidosis have no involvement of other organs.
- Lesions may be non-specific or specific based on the presence or absence of noncaseating granuloma on histopathologic examination.
Non-specific lesions include:
- Erythema nodosum: the most common non-specific lesion
- This presents with tender erythematous nodules mostly on the shins; often accompanied by arthritis in the ankles, elbows, wrists, and hands (Löfgren syndrome)
- Nummular eczema
- Erythema multiforme
- Calcinosis cutis (deposition of calcium salts within the skin)
- Pruritus (itch).
Specific lesions show granulomas on histology (microscopic examination of a skin biopsy) and include:
- Lupus pernio: large bluish-red and dusky purple infiltrated nodules and plaque-like lesions on nose, cheeks, ears, fingers and toes (not chilblains), associated with a chronic and refractory course of sarcoidosis
- Skin plaques: purple-red or brown, thickened, circular skin lesions, associated with a chronic course of the disease
- Papules and papulonodules – firm and non-scaly, may be flesh-coloured, yellow-brown, red-brown, purple-brown, or hypopigmented
- Subcutaneous nodules (Darier-Roussy disease)
- Infiltration (thickening) of old scars (scar sarcoidosis) and sarcoid in tattoos
- Ichthyosiform
- Necrobiosis-like lesions
- Mucosal involvement — buccal mucosa, gingiva, hard palate, tongue, posterior pharynx and salivary glands
- Erythroderma
- Alopecia
- Nail sarcoidosis — thinning, brittle and thickened nails, pitting, ridging, trachyonychia, hyperpigmentation, clubbing or pseudo-clubbing, destruction of the nail plate, and scarring.
Eye
Any part of the eye can be involved:
- Uveitis: the most common form of ocular involvement, may affect 20–30% of patients with sarcoidosis, results in blurred vision, watery eyes, and photophobia
- Scleritis/episcleritis
- Iris nodules
- Retinochoroiditis
- Conjunctivitis
- Lacrimal gland involvement — can cause sicca syndrome
- Optic nerve involvement leading to optic neuropathy, prognosis is not favourable and permanent impaired visual acuity occurs in about one-third of the patients
- Ocular nerve palsy can occur from sarcoid involvement of the 3rd, 4th, and 6th cranial nerves
- Proptosis (protruding eyeball).
Uncommonly, cataracts, glaucoma, and blindness can result.
Liver
- Up to one third have changes in their liver enzyme levels. Alkaline phosphatase is more consistently elevated than aminotransferases in hepatic sarcoidosis.
- Hepatic involvement may present as hepatomegaly, fatigue, right upper quadrant abdominal pain with pruritus (5–15%), fever, jaundice, and weight loss (less than 5%).
Heart
- Cardiac involvement is reported in approximately 3–39% of patients with systemic sarcoidosis.
- May present with heart failure, arrhythmias, or syncope.
- Cardiac sarcoidosis is much more common in the Japanese than in other races. In Japan, the main cause of mortality in sarcoidosis patients is cardiac involvement, which is responsible for 77% of deaths in people with sarcoidosis.
Nervous system
- Neurological involvement is reported in 3–10%.
- The most frequently affected sites include the cranial nerves (55%), the brain parenchyma (20–45%), the meninges (12–40%), and the spinal cord (18–26.5%).
- May result in neurological deficits, seizures, encephalopathy, headache, confusion, and malaise.
Musculoskeletal system
- Joint involvement, also known as sarcoid arthropathy, occurs in 6–35%.
- There is asymptomatic bone involvement in 3–13%.
- Sarcoid myopathy occurs in <3%.
- Arthritis is most commonly acute, resulting in swelling of the lower legs and tenderness of ankles, knees, and fingers.
- Chronic (long term) sarcoid arthritis is rare (7%).
- Digit swelling (dactylitis).
Calcium metabolism
- Hypercalcemia affects 7–18% of patients with sarcoidosis due to overproduction of vitamin D by sarcoid granulomas.
- Kidney stones (nephrolithiasis) may result from abnormal calcium metabolism (10–14%) and hypercalciuria.
Kidneys
- Granulomatous interstitial nephritis is the classic renal pattern of sarcoidosis
- Clinically evident interstitial nephritis is observed in 0.7 to 4.3% in clinical studies.
Sarcoidosis
How is sarcoidosis diagnosed?
The diagnosis of sarcoidosis is based on three major criteria:
- Consistent and adequate clinical presentation
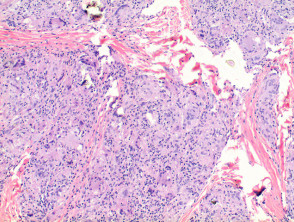
- Demonstration of the presence of non-caseating granulomas in one or more tissue samples
- The exclusion of other causes of granulomatous disorders.
There is no established “gold standard” investigation, however the following may be performed when sarcoidosis is suspected; results must be taken in combination with the history and examination.
- Chest x-ray
- Bilateral hilar lymphadenopathy, disseminated nodules in the lungs.
- Lung function
- Assess pulmonary involvement and disease severity.
- Granulomas and fibrosis of lung tissue reduce lung capacity and disturb the normal flow of gasses.
- Blood
- Mild anaemia occurs due to granulomatous bone marrow involvement, or chronic disease state.
- Lymphopenia.
- Increase in serum calcium levels and abnormal liver function tests often accompany sarcoidosis.
- Serum angiotensin-converting enzyme (ACE) indicates total granuloma load. Higher in sarcoidosis patients but not specific to sarcoidosis.
- Tissue biopsy (for the presence of granuloma)
- Lungs, lymph node, skin, salivary gland, conjunctiva
- Bronchial biopsy — detect pulmonary involvement, (Endobronchial ultrasound-guided transbronchial needle aspirate [EBUS-TBNA], Trans and endobronchial Biopsy)
- Microscopic examination of specimens of organ tissue can show granulomas and confirm a diagnosis. Multiple biopsies may be necessary.
- Specific pathological features of sarcoidosis are often present in skin biopsy samples of the condition.
- Ophthalmologic examination
- Used to detect orbital and eyelid granulomas
- Other tests
- High-resolution CT — differentiation of sarcoidosis from other pulmonary conditions
- FDG-PET — highly sensitive to detect cardiac and pulmonary involvement
- ECG — ectopic beats, arrhythmias
- MRI — detect neurological involvement, spinal cord, meninges, skull vault, and pituitary lesions
- Kveim test — injection of sarcoidal spleen, biopsied to determine whether granulomas have formed (not available in some countries)
- Liver and kidney function tests
- 24-hour urinary calcium excretion
- Angiotensin-converting enzyme
- TB testing: negative in sarcoidosis
- Skin biopsy of sarcoidosis — specific skin lesions has good sensitivity for demonstrating noncaseating granuloma (90% in one study)
What is the differential diagnosis?
The differential diagnosis includes:
- Lymphoproliferative disorders such as Hodgkin’s lymphoma
- Infectious diseases including leishmaniasis, toxoplasmosis, and tuberculosis
- Granulomatosis with polyangiitis, granulomatosis with eosinophilia and polyangiitis (Churg-Strauss syndrome).
What is the treatment for sarcoidosis?
For most patients with sarcoidosis, no treatment is required. Symptoms are not usually disabling and tend to disappear spontaneously. Surveillance for 3–12 months is typically advised to determine the overall course of the disease. Treatment is indicated only when symptoms are disabling and/or the granulomatous inflammation is causing life-threatening organ involvement.
- Oral corticosteroids are first-line treatment; they provide symptomatic relief and reverse organ dysfunction, but treatment risks should be taken into account.
- Prednisolone is often initiated at 0.5–0.75 mg/kg daily for 4 weeks and tapered by 10 mg every 4 weeks, depending on disease response. However, this dose may be too high, and 20 mg of prednisone can be used as an alternative.
- Corticosteroid-sparing regimens can also be used as second-line therapy. For example, azathioprine, methotrexate, mycophenolate mofetil, cyclosporin, cyclophosphamide, leflunomide, and hydroxychloroquine for symptomatic relief.
- Biological agents are considered third-line therapy for patients with refractory disease.
- The use of anti-TNF antibodies such as infliximab or adalimumab has shown some therapeutic benefits.
- Ustekinumab and canakinumab were recently evaluated with mixed results. In a recent study, neither ustekinumab nor golimumab demonstrated efficacy in pulmonary sarcoidosis. However, trends towards improvement were observed with golimumab in skin sarcoidosis.
- Success in individual cases has been reported with allopurinol, isotretinoin, leflunomide, pentoxifylline, thalidomide, and JAK inhibitors (eg, tofacitinib).
- Other agents such as roflumilast, apremilast, and nicotine patches are currently being investigated by ongoing clinical trials.
Most will recover in a short time frame whilst a small number do not recover after 2–5 years. These chronic patients frequently need long-term treatment.
What is the treatment of cutaneous sarcoidosis?
Erythema nodosum, the common nonspecific cutaneous lesion, is usually self-limiting. Short-course nonsteroidal anti-inflammatory drugs (NSAIDs) or glucocorticoids may be prescribed to treat pain and discomfort.
Sarcoidosis-specific cutaneous lesions can improve spontaneously. Cutaneous lesions are treated only if they cause significant cosmetic disfigurement, psychological effects, or if the lesions are progressive. Treatment is as follows:
- Local glucocorticoid treatment: either topical or intralesional, is first-line therapy. Ultrapotent formulations, such as clobetasol and halobetasol propionate, are generally required.
- Cases of lupus pernio achieved considerable improvement with halobetasol propionate 0.05% ointment twice daily for 10 weeks.
- Oral glucocorticoids or hydroxychloroquine: used for extensive cutaneous disease or second-line of therapy.
- Response is generally favourable, with complete resolution seen within 2 years in most patients.
- Hydroxychloroquine has been suggested as quite effective for cutaneous sarcoidosis, but not considered highly effective for pulmonary disease
- Addition of alternative oral systemic drugs: considered if no response to systemic glucocorticosteroids.
- Most commonly: hydroxychloroquine, chloroquine, and methotrexate.
- Biologic agents: reserved for patients where all other treatments have failed.
- Most commonly: Infliximab, which has the most robust data.
- Laser surgery has been used in treating disfiguring skin plaques and lupus pernio.
How serious is sarcoidosis and what is the prognosis?
Two-thirds of patients report a self-remitting disease within 12 to 36 months. The remainder of patients may follow a chronic course (10 to 30% require prolonged treatment). With correct diagnosis and proper management, most patients with sarcoidosis continue to lead a normal life.
Cutaneous sarcoidosis usually has a more prolonged course. Papules and nodules tend to resolve over months or years. Plaques may be more resistant. Lupus pernio is often present in patients with chronic sarcoidosis and is associated with involvement of the upper respiratory tract, advanced lung fibrosis, bone cysts, and eye disease.
Factors associated with poor prognosis include: ethnicity (particularly African American and Afro Caribbean origins), age over 40 years at presentation, lupus pernio, chronic uveitis, CNS involvement, cardiac involvement, severe hypercalcemia, nephrocalcinosis, and radiographic stages III and IV.
In Western countries, most sarcoidosis deaths are due to advanced pulmonary fibrosis leading to respiratory failure and/or pulmonary hypertension and less commonly, cardiac and CNS sarcoidosis or portal hypertension. In addition to treatment-related mortality, less common causes of death include lymphoma and haemoptysis due to mycetoma.