What is a leg ulcer?
A chronic leg ulcer is defined as full thickness skin loss for > 3 months. At times, it can be difficult to determine the correct diagnosis of a leg ulcer. At least 15% of leg ulcers are of mixed aetiology. It is essential to take a thorough medical history and to examine the patient carefully, looking for local and systemic clues to the diagnosis.
Contributing factors to leg ulceration
Whatever the primary cause of the ulcer, there are often other factors that contribute to the poor healing of ulcers. These include:
- Increased age and immobility or infirmity
- Vascular disease
- Lower leg oedema
- History of deep venous thrombosis
- Previous surgery
- Biofilm
- Obesity
- Diabetes
- Smoking
- Alcohol
- Malnutrition
- Blood dyscrasia: sickle-cell disease, thalassaemia, thrombocythaemia, polycythaemia and others
- Hyperlipidaemia
- Renal failure
- Chemotherapy
- Radiotherapy
- Genetic disease, eg, Ehlers Danlos syndrome
Immediate cause of ulceration
An ulcer often begins with:
- Injury – look out for a foreign body. Trauma is a very common cause of chronic ulcer.
- Pressure – the site requires on-going protection from injury
- Acute infection – staphylococcus, streptococcus, other, or mixed
Chronic infection can also be responsible for ulceration, particularly:
- Tropical ulcer
- Atypical mycobacteria especially M ulcerans, the cause of Buruli ulcer
- Leprosy (neuropathic ulceration)
- Cutaneous tuberculosis
- Deep fungal infection
- Leishmaniasis
Infection is identified by swabs and biopsy samples sent for bacterial and fungal microscopy and culture.
Infections causing leg ulcers
Common reasons for leg ulceration
Chronic venous insufficiency (70%)
- Stasis ulcer is found on the lower leg, most often above the medial or lateral malleolus
- Often relatively painless, sometimes painful if infected
- Brown haemosiderin staining of the lower leg is commonly present
- May also have venous eczema, oedema, lipodermatosclerosis
Ulceration due to venous insufficiency
Chronic arterial insufficiency (10%)
- Arterial ulcer is found on feet, heel or toe
- Painful, especially when elevated
- Punched out ulcer
- Cold, white, shiny, hairless skin
- Ankle-brachial pressure index < 0.9
- Pulses reduced or absent
Neuropathic ulceration
- A neuropathic ulcer arises in numb skin
- Unnoticed trauma causes painless ulceration
- Ulceration is often at a pressure point
Neuropathic ulceration
Diabetic ulcer
- Diabetic foot ulcers are usually of mixed aetiology
- Frequently secondarily infected
- Ulceration is a common precursor to amputation in diabetics
Diabetic ulceration (mixed aetiology)
Pressure ulcers
- Pressure or decubitus ulcers are caused by unrelieved pressure
- Occur on bony prominences, eg, sacrum, heel
- Often infected, leading to septicaemia and osteomyelitis
Pressure sore
Hypertensive ulcer
- Martorell ulcer is due to uncontrolled hypertension
- May contribute to diabetic ulcer
- Often on the back of the lower leg
- Extremely painful
- Biopsy shows thickened arteriolar walls
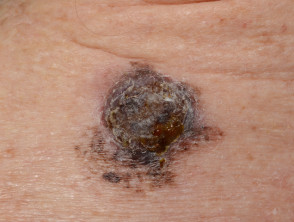
Skin cancer
- Skin cancer presents as a slowly-growing plaque or nodule
- Most skin cancers are on sun-exposed sites
- Ulceration occurs earlier in basal cell carcinoma than in squamous cell carcinoma
- Biopsy is diagnostic
Ulcerated skin cancers
Inflammatory causes of leg ulceration and vascular occlusion
Inflammatory causes of leg ulceration can be difficult to diagnose and difficult to treat.
If considering an inflammatory cause of leg ulceration, diagnostic tests may involve:
- Deep skin biopsy of ulcer edge for histology, fungal/mycobacterial culture, direct immunofluorescence
- CBC, CRP/ESR, c/p-ANCA, metabolic panel, protein electrophoresis and immunoglobulins, coagulation studies, antiphospholipid antibody, cryoglobulins, cryofibrinogen, ANA, complement, hepatitis B/C serology, blood cultures
- Urinalysis
- Chest X-ray, colonoscopy, echocardiography, arterial and venous studies
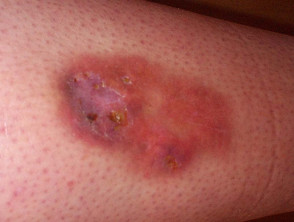
Pyoderma gangrenosum
- Pyoderma gangrenosum is an autoinflammatory disease associated with inflammatory bowel disease, rheumatoid arthritis, myeloid dysplasia, gammopathy
- Rapid wide and deep enlargement of the ulcer is typical
- Very painful
- Undermined necrotic edge with pustules and necrotic base
- Pathergy: surgery risks enlargement of ulcer
- Heals with cribriform scarring
- Histology nonspecific or neutrophilic infiltrate
Pyoderma gangrenosum
Small vessel vasculitis
- Small vessel vasculitis (from many causes) results in palpable purpura with haemorrhage, ischaemia and infarction
- Vasculitic lesions can ulcerate
- Ulcers mostly occur on lower legs and ankles
- Biopsy shows leukocytoclastic vasculitis
Small vessel vasculitis
Medium vessel vasculitis
- Medium vessel vasculitis (eg, polyarteritis nodosa, granulomatosis with polyangiitis) results in livedo reticularis, arterial nodules, and gangrene
- Painful, punched-out, irregular ulcers typically affect lower legs
- Biopsy shows vasculitis of medium-sized vessels
Medium vessel vasculitis: polyarteritis nodosa
Rheumatoid ulceration
- Rheumatoid ulceration is multifactorial: venous and arterial disease, diabetes, vasculitis and unknown
- Very painful
- Usually causes an ulcer near the ankle
- May have other signs of vasculitis: small nail fold infarcts, digital ischaemia, scleritis, mononeuritis multiplex, pericarditis, pleuritis, fever, weight loss
- Biopsy from ulcer edge may detect medium-vessel vasculitis
Rheumatoid ulcers
Necrobiosis lipoidica
- Necrobiosis lipoidica is associated with type 1 diabetes in 50%
- Yellow-red, atrophic and telangiectatic plaques
- Plaques are mainly found on shins
- Ulceration is very resistant to treatment
- Biopsy shows atrophic epidermis, dermal necrobiotic collagen
Ulcerated necrobiosis lipoidica
Systemic sclerosis
- Systemic sclerosis causes fibrin-occlusive vasculopathy
- 50% associated with antiphospholipid antibodies
- Often results in bilateral, painful ulcers lower leg
- Painful ischaemic digital ulcerations are also common, due to Raynaud phenomenon
Ulcerated systemic sclerosis
Livedoid vasculopathy
- Livedoid vasculopathy is associated with coagulation disorders
- Small painful superficial ulcers on ankles
- Heals with atrophie blanche
Livedoid vasculopathy
Warfarin-induced skin necrosis
- Warfarin- induced skin necrosis follows the initiation of warfarin 3–10 days earlier
- Sudden onset of ecchymosis progresses to a necrotic ulcer
- Biopsy shows intravascular thrombi without vasculitis
Heparin-induced necrosis
- Heparin-induced necrosis follows the initiation of heparin 4–12 days earlier
- Associated with heparin-induced thrombocytopenia in most but not all patients
- Biopsy shows intravascular clumps of platelets
Other coagulopathy
- Antiphospholipid syndrome, protein S and protein C deficiency and others
- Acute thrombosis progresses to a necrotic ulcer
- Biopsy shows intravascular thrombi without vasculitis
Cholesterol embolism
- Cholesterol emboli are often the consequence of an endovascular surgical procedure or initiation of anticoagulant therapy (days to months later)
- Livedo reticularis, purpura, cyanosis, blue toes, digital gangrene, painful subcutaneous nodules
- Systemic symptoms include fever, weight loss, myalgia, anaemia, renal failure
- Biopsy reveals biconvex needle-like cleft in vessels on histology
Cholesterol emboli
Septic emboli
- Septic emboli are due to endocarditis or septicaemia; various organisms are involved
- Purpura, pustules, haemorrhagic bullae, splinter haemorrhages in nails
- Ulcers usually small and irregular, often on feet
- Biopsy shows small blood vessel occlusion + small vessel vasculitis (immune complex negative)
Septic emboli
Calciphylaxis
- Calciphylaxis is associated with chronic renal failure and secondary hyperparathyroidism, obesity, liver disease, systemic corticosteroids, diabetes and coagulation defects
- Occurs on lower limbs, breasts, abdomen, buttocks
- Painful, deep, ulceration preceded by tender, retiform purpura
- Biopsy shows calcification of vessel walls, thrombosis and infarction
Calciphylaxis
Cryofibrinogenaemia
- Cryofibrinogenaemia is associated with malignancy, diabetes, connective tissue disease, infection but is more often idiopathic
- Presents with livedo reticularis, purpura, ecchymoses, malaise and fever
- Sudden onset of painful ischaemic ulceration
- Plasma cryofibrinogen is elevated
- Biopsy shows small and medium vessel vasculitis
Cryoglobulinaemia
- Cryoglobulinaemia is associated with connective tissue disease, haematological malignancies, hepatitis
- Systemic symptoms include arthralgia, weakness
- Purpura triggered by cold exposure or prolonged standing
- Cryoglobulins detected in serum
- Biopsy shows small and medium vessel vasculitis
Cryoglobulinaemia
Levamisole-adulterated cocaine vasculopathy
Levamisole-adulterated cocaine can result in a combination of:
- Occlusive vasculopathy
- Small vessel vasculitis