What is a rheumatic disease?
Many autoimmune connective tissue diseases and vascular conditions in rheumatology have cutaneous manifestations.
- Skin signs are useful in the diagnosis of rheumatic disease, as they often precede systemic symptoms.
- They can also act as a prognostic marker and predict systemic involvement.
Rheumatic diseases described on this page are:
- Cutaneous lupus erythematosus
- Dermatomyositis
- Systemic sclerosis
- Scleroedema
- Scleromyxoedema
- Rheumatoid arthritis
- Systemic-onset juvenile arthritis
- Relapsing polychondritis
- Psoriatic arthritis
- Osteoarthritis
- Vasculitis.
Cutaneous lupus erythematosus
About 25% of patients with systemic lupus erythematosus (SLE) initially present with skin involvement. It is important to correctly classify cutaneous lupus erythematosus (CLE), as it helps determine the underlying type and severity of SLE. About 5–10% of patients with CLE develop SLE, and CLE is associated with less severe forms of SLE.
Skin manifestations of lupus erythematosus are commonly divided into lupus erythematosus–specific and non–specific disease. Note that four of the nine American College of Rheumatology criteria for SLE are skin signs (ie, malar/butterfly rash, discoid plaques, photosensitivity, and oral ulcers).
Lupus erythematosus–specific disease
Acute cutaneous lupus erythematosus
Forms of acute CLE include the following:
- Localised acute CLE — this presents with malar or 'butterfly' rash (symmetrical erythema and oedema of the cheeks, forehead, chin, and V of the neck but sparing the nasolabial folds or 'smile lines')
- Generalised acute CLE — this presents with a widespread exanthematous eruption on the extensor surfaces, trunk, sun-exposed areas, and hands (but sparing the knuckles)
- Toxic epidermal necrolysis-like acute CLE — this is a life-threatening variant of acute CLE that presents with a massive epidermal injury; it occurs predominantly on sun-exposed skin and has a gradual, insidious onset, unlike toxic epidermal necrolysis.
Acute CLE is typically triggered or exacerbated by exposure to ultraviolet (UV) radiation. On recovery, there may be postinflammatory hyperpigmentation without scarring.
Malar rash of systemic lupus erythematosus
Subacute cutaneous lupus erythematosus
Subacute cutaneous lupus erythematosus (SCLE) starts as macules or papules that progress to hyperkeratotic plaques. SCLE is photosensitive so plaques usually occur on sun-exposed skin; these plaques do not lead to scarring but can result in postinflammatory hyperpigmentation or hypopigmentation. SCLE should be monitored to exclude any progression to SLE.
Forms of SCLE include:
- Annular SCLE — this subtype presents with slightly raised red lesions with central clearing
- Papulosquamous SCLE — this subtype presents with eczematous or psoriasis-like lesions on sun-exposed skin.
Subacute cutaneous lupus erythematosus
Chronic cutaneous lupus erythematosus
Chronic CLE is not as photosensitive as acute CLE or SCLE. Forms of chronic CLE include:
- Discoid lupus erythematosus (DLE) — this affects the face, outer ears, neck, sun-exposed areas and lips, and presents with discoid plaques (erythematous, well-demarcated plaques covered by scale) that become hyperkeratotic, leading to atrophy and scarring; there is follicular involvement, causing both reversible and irreversible (scarring) alopecia (hair loss); dyspigmentation of the peripheries is also common in certain ethnicities (Asian, Indian)
- Hypertrophic or verrucous lupus erythematosus — this is a rare form of CLE presenting with severe hyperkeratosis of the extensor surfaces of the arms, upper back and face; it has overlapping features with lichen planus.
- Mucosal lupus erythematosus — this affects 25% of patients with CLE; most commonly, painless erythematous patches on the oral mucosa develop into chronic plaques that can centrally ulcerate and also affect nasal, conjunctival and genital mucosa; oral lupus erythematosus rarely degrades to oral cancer (squamous cell carcinoma).
Discoid lupus erythematosus
Drug-induced lupus erythematosus
Many drugs are thought to induce SLE and drug-induced lupus erythematosus often includes cutaneous signs. Drugs that induce lupus erythematosus include:
- Hydralazine
- Isoniazid
- Chlorpromazine
- Procainamide
- Phenytoin
- Minocycline
- Anti–tumour necrosis factor medications.
Drug-induced cutaneous lupus
Rarer types of lupus erythematosus
The rarer types of lupus erythematosus include:
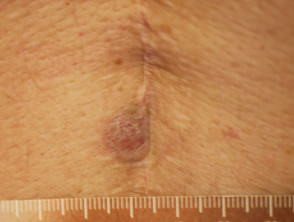
- Lupus profundus/lupus panniculitis — this is a rare form of chronic CLE with firm nodules in the lower dermis and subcutaneous tissue that causes lipodystrophy; some use the term lupus panniculitis to refer to subcutaneous involvement only, and lupus profundus when there is a combination of lupus panniculitis with DLE.
- Chilblain lupus erythematosus — this presents with purple-red patches, papules and plaques on toes, fingers and face, and is associated with nail fold telangiectasia; it is precipitated by exposure to the cold, so often presents in winter.
- Lupus erythematosus tumidus —this is a variant of chronic CLE with succulent or indurated erythematous plaques without surface change.
Rare forms of chronic cutaneous lupus erythematosus
Lupus erythematosus — non–specific disease
Lupus erythematosus-nonspecific disease can relate to SLE or another autoimmune disease, but nonspecific cutaneous features are most often associated with SLE.
Common cutaneous features seen include:
- Photosensitivity — this is an abnormal response to UV radiation that is present in 50–93% of patients with SLE
- Mouth ulcers — these are present in 25–45% of patients with SLE
- Non–scarring hair loss in SLE — presenting as coarse, dry hair with increased fragility (also referred to as 'lupus hair').
Cutaneous vascular disease is also common. Forms of cutaneous vascular disease include:
- Raynaud phenomenon — this presents with focal ulceration in the fingertips and periungual areas that can cause pitted scarring, haemorrhage and other nail fold complications
- Vasculitis — leukocytoclastic vasculitis: urticarial vasculitis presenting with tender papules and plaques over bony prominences; and medium or large vessel vasculitis can occur, presenting with purpuric plaques with stellate borders, often with necrosis and ulceration or subcutaneous nodules
- Thromboembolic vasculopathies — these may have a similar clinical presentation to vasculitis, but vessel occlusion is due to blood clots
- Livedo reticularis — characterised by net-like blanching red-purple rings that commonly arise on the lower limbs
- Erythromelalgia — characterised by burning pain in the feet and hands, and with macular erythema; it is associated with heat exposure.
Vascular disease in lupus erythematosus
Other symptoms include:
- Cutaneous mucinosis — characterised by indurated papules, nodules, or plaques on the trunk or arms
- Lupus nail dystrophy — presenting as nail pitting, ridging, leukonychia, onycholysis, and red lunula
- Spontaneous chronic urticaria
- Lichen planus
- Acanthosis nigricans
- Sclerodactyly (spindle-shaped fingers)
- Erythema multiforme
- Cutis laxa
- Rheumatoid nodules.
Dermatomyositis
Dermatomyositis (also known as idiopathic inflammatory myopathies) is a heterogeneous group of autoimmune disorders affecting the skin and musculature.
Skin signs are critical in diagnosing and classifying dermatomyositis:
- Amyopathic dermatomyositis — this involves skin changes without muscle or other systemic involvement for more than 6 months.
- Classic dermatomyositis — this is more common and results in skin and muscle disease.
Two hallmark skin signs of dermatomyositis help differentiate it from CLE; these are:
- Gottron papules — these are violaceous macules over the knuckles and in periungual areas; they often have a depressed centre that is white or atrophic
- Gottron sign — this refers to symmetrical violaceous macules, sometimes with oedema, over the knuckles, elbows, or knees.
Classic skin signs of dermatomyositis include:
- Periorbital macules — these are violaceous, erythematous ('heliotrope') macules of the eyelids and periorbital tissue, presenting with or without oedema
- Periungual telangiectasia
- Macules over the hands and fingers — these present with symmetric erythema on the dorsum of hands and fingers, the extensor surface of arms, deltoids, posterior shoulders, V area of the neck, central forehead, face and scalp
- Mechanic’s hand (a sign of antisynthetase syndrome) — this is characterised symmetrical chronic eczema-like scaling affecting the hands, especially along the ulnar side of the thumb and radial side of the fingers.
Other skin signs of dermatomyositis include:
- Poikiloderma — this is a combination of violaceous erythema, dyspigmentation, telangiectasia and atrophy of the skin; most commonly over the shoulders, back, buttocks, V of neck and chest
- Calcinosis cutis — presenting as painful irregular nodules at sites of friction and trauma, such as the elbows, knees and fingers.
Dermatomyositis
Systemic sclerosis
Systemic sclerosis is a multi-system form of scleroderma with hallmark skin signs. It is associated with a high mortality and morbidity rate. The clinical features of systemic sclerosis are diverse and affect multiple organs in the body.
Two important skin signs of systemic sclerosis are Raynaud phenomenon and skin sclerosis; these signs help classify the disease into the following subsets.
- Localised systemic sclerosis — features of which involve pre-existing chronic Raynaud phenomenon for a period of years and skin sclerosis (scleroderma) affecting the face, neck, and extremities, while sparing proximal body sites
- CREST syndrome — this involves:
- Calcinosis
- Raynaud phenomenon
- (o)Esophageal symptoms
- Sclerodactyly
- Telangiectasia.
- Visceral disease — this may begin after a long period of Raynaud disease and can involve pulmonary arterial hypertension, pulmonary fibrosis, and gastrointestinal tract involvement
- Diffuse systemic sclerosis — features of which include Raynaud phenomenon of recent onset and proximal scleroderma affecting upper arms, thighs, chest and abdomen; there is an acute onset with inflammatory features in the first 24 months of disease; pulmonary fibrosis, cardiac disease and renal crisis are also common
- Overlapping systemic sclerosis — these patients have features of scleroderma with another autoimmune rheumatic disease, such as dermatomyositis or polymyositis, SLE, Sjögren disease, vasculitis, or polyarteritis.
Cutaneous signs of systemic sclerosis
Scleroedema
Scleroedema is a rare disease caused by excessive mucin and collagen production. It is associated with preceding infection, diabetes and paraproteinaemia. Skin signs accompanying the disease include:
- Non-pitting induration of the neck, shoulders, and upper back — appearing with acute onset
- Waxy smooth skin with prominent follicular ostia.
Scleromyxoedema
Scleromyxoedema is a rare disease caused by excessive mucin production and fibrocyte hyperplasia. It is associated with paraproteinaemia.
- Scleromyxoedema is associated with generalised lichenoid eruption — presenting as confluent papules scattered on the trunk and extremities
- Discrete papular scleromyxoedema — presents with discrete papules on the trunk and extremities
- Lichen myxoedematosus is a localised form of scleromyxoedema with nodules
- Lichenoid plaques and urticarial plaques may also occur.
Scleromyxoedema
Sjögren syndrome
Sjögren syndrome is a systemic autoimmune disorder that primarily reduces the function of the sweat glands and mucous glands, causing sicca symptoms. Sjögren syndrome is much more common in women than in men.
Mucosal signs of Sjögren syndrome include:
- Xerosis (dryness of mucous membrane)
- Xerostomia (dry mouth) — this predisposes to angular cheilitis
- Dry eye.
Skin signs of Sjögren syndrome include:
- Eyelid dermatitis
- Vaginal dryness — resulting in burning and painful sex
- Diffuse hair loss
- Vitiligo
- Raynaud phenomenon — this is the most common sign of Sjögren syndrome and can precede sicca symptoms by many years.
- Cutaneous vasculitis commonly presents with non-palpable purpura — crops of round pink lesions that turn purple and then brown
- Dermal vasculitis presents with palpable purpura and commonly occurs on the buttocks and lower limbs
- Urticarial vasculitis — is characterised by erythematous urticated weals that each last more than 24 hours and resolve with hyperpigmentation
- Necrotising vasculitis — presents initially with palpable purpura on the lower limbs that ulcerate and form scars in 1–4 weeks.
- Annular erythema — presenting with annular erythematous plaques with central clearing; this may be found in Asian patients with anti-Ro/SSA antibodies
- Erythema nodosum
- Erythema multiforme.
Vasculitis in Sjogren syndrome
Rheumatoid arthritis
Rheumatoid arthritis is a systemic autoimmune inflammatory disorder that causes debilitating symmetrical polyarthritis and other manifestations. One of the seven criteria for RA is the presence of rheumatoid nodules. Its skin signs can be divided into rheumatoid arthritis-specific and nonspecific signs.
Rheumatoid arthritis-specific skin signs
- Rheumatoid nodules — these are subcutaneous, firm, painless lesions over the extensor surfaces of the skin as well as in the heart, lungs, and muscles in 25% of cases; they may be complicated by ulceration, bursitis, synovial rupture, and gangrene.
- Accelerated rheumatoid nodulosis — presenting as painful nodules mainly on the hands; associated with methotrexate therapy in patients with rheumatoid arthritis.
- Rheumatoid vasculitis — this is a late-stage presentation of rheumatoid arthritis characterised by purpura, splinter haemorrhage, nail-fold infarcts, and peripheral neuropathy that is more common in men; these patients should be started on aggressive therapy for rheumatoid arthritis.
- Rheumatoid neutrophilic dermatosis — this is a rare sign in severe seropositive rheumatoid arthritis presenting as asymptomatic red urticated papules and plaques on the forearms and hands; it resembles acute febrile neutrophilic dermatosis (also known as Sweet syndrome).
Other signs of vasculitis associated with rheumatoid arthritis include:
- Erythema elevatum diutinum
- Livedo reticularis
- Gangrene
- Digital infarcts
- Urticarial vasculitis
- Atrophie blanche
- Haemorrhagic blisters
- Necrotising granulomatous vasculitis.
Rheumatoid arthritis-nonspecific skin signs
Rheumatoid arthritis-nonspecific skin signs include:
- Pyoderma gangrenosum — presenting as tender erythematous or violaceous papules that rapidly develop into necrotic ulcers with ragged swollen edges, usually on the legs
- Palisaded neutrophilic and granulomatous dermatitis (also known as Winkelmann granuloma) — characterised by symmetrical papules, nodules, or plaques on the extensor surfaces of the elbows and fingers, often with a central umbilication and crusts.
- Interstitial granulomatous dermatitis — presenting as well-demarcated papules or plaques that can coalesce into linear cords; these papules or plaques are typically on the trunk and proximal limbs.
Other skin signs arising in rheumatoid arthritis include:
- Cutaneous atrophy
- Palmar erythema
- Onycholysis
- Periungual erythema
- Yellow nail syndrome
- splinter haemorrhage
- Hyperpigmentation
- Erythromelalgia
- Erythema multiforme
- Vitiligo
- Alopecia areata.
Cutaneous signs of rheumatoid arthritis
Systemic-onset juvenile arthritis
Systemic–onset juvenile arthritis is a form of juvenile idiopathic arthritis characterised by high fevers, arthritis, and skin signs (in 95% of cases). Lymphadenopathy, myalgia, and abdominal pain may be present. Key signs include:
- Macular exanthema — this presents as non-pruritic and transient exanthema in 90% of acutely febrile patients with discrete macules often occurring on the trunk; koebnerisation is common
- Rheumatoid nodule-like lesions — characterised by nodules on the extensor surfaces, that are clinically and histologically indistinguishable from rheumatoid arthritis.
Relapsing polychondritis
Relapsing polychondritis is a rare multisystem autoimmune disease, often associated with an autoimmune or haematological condition. Skin signs in relapsing polychondritis are nonspecific; they are not diagnostic criteria, nor are they associated with disease severity.
Hallmark signs of relapsing polychondritis are:
- Auricular inflammation — presenting as ear cartilage swelling, erythema and pain in 85% of cases
- Nasal cartilage inflammation — characterised by nasal pain, rhinorrhoea (runny nose), and epistaxis in 65% of cases
- Saddle-nose deformity.
Other skin signs occurring in relapsing polychondritis include:
- Non-specific vasculitic signs — these are present in 12% of patients with relapsing polychondritis
- Nodules on the limbs
- Purpura
- Oral aphthous ulcers
- Papules
- Livedo reticularis
- Ulcers
- Distal necrosis.
Relapsing polychondritis
Psoriatic arthritis
Psoriatic arthritis is a form of spondyloarthropathy that can be associated with psoriasis. Psoriasis typically presents with red scaly plaques on the scalp and the extensor surfaces as well as nail psoriasis. There are subtypes of psoriasis with specific skin signs; these include:
- Chronic plaque psoriasis (psoriasis vulgaris) — presenting as sharply demarcated plaques with silvery scale, typically involving the elbows, knees, lower back, scalp and umbilicus.
- Guttate psoriasis — this presents as an acute eruption of papules and plaques less than 1 cm in size; it starts on the trunk and spreads to the proximal limbs
- Nail psoriasis — this affects 60–90% of patients with psoriatic arthritis and presents with oil spots, pits, onycholysis and onychodystrophy (malformation of the nails)
Psoriasis
- Psoriatic erythroderma — this is a potentially life-threatening generalised erythema of the entire skin
- Pustular psoriasis — consisting of localised palmoplantar pustulosis presenting as sterile pustules on palms and soles or generalised pustular psoriasis characterised by an acute febrile eruption over the trunk and limbs.
Uncommon forms of psoriasis
Osteoarthritis
Osteoarthritis is a degenerative form of arthritis that causes discomfort, pain and stiffness in other joints of the hands, the knees, hips, and spine. Many patients with osteoarthritis have Heberden and Bouchard nodes.
Vasculitis
Systemic vasculitis is a heterogeneous group of disorders presenting with inflammation of the blood vessel walls. The skin and blood vessels have a close anatomical and physiological relationship; hence, skin signs are common in vasculitis. These include:
- Palpable purpura
- Livedo reticularis
- Infiltrative erythema
- Ulcers
- Digital ischaemia.
These skin signs prompt an investigation for any systemic involvement of vasculitis. However, the skin signs alone are not sufficient for the diagnosis of a specific condition.
Cutaneous signs of vasculitis
Small vessel vasculitis
Small vessel vasculitis presents with palpable purpura, usually more pronounced on gravity-dependent areas, with associated oedema.
Forms of small vessel vasculitis and their associated skin signs include:
- Granulomatosis with polyangiitis — associated with antineutrophil cytoplasmic antibodies (ANCAs), this presents as potentially lethal necrotising granulomatous inflammation and vasculitis; the skin signs are highly variable and include palpable purpura, deep inflammatory indolent masses, gingival enlargement, ulcers, panniculitis and nodules, and pyoderma gangrenosum-like ulcers.
- Eosinophilic granulomatosis with polyangiitis — another ANCA-associated vasculitis; skin signs occur in 50% of cases and comprise palpable purpura, macules, papules, and nodules on the extensor surfaces; rarely, facial oedema, ulcers, livedo reticularis, and deep pannicular vasculitis also occur.
- Microscopic polyangiitis — this is another ANCA-associated vasculitis; its skin signs typically manifest with consist of purpura and splinter haemorrhage
- Cryoglobulinaemic vasculitis — cryoglobulins are circulating immunoglobulins complexed to other immunoglobulins or proteins that reversibly precipitate (leach) out of the blood in the cold; type I cryoglobulinaemia occurs in single monoclonal immunoglobulins while mixed type cryoglobulinaemia (types II and III) results in vasculitis with glomerulonephritis (inflammation of kidneys); purpura at distal sites (fingers and toes) is a hallmark sign
- Type I cryoglobulinaemia — skin signs include non-inflammatory purpura, Raynaud phenomenonlivedo reticularis, ulceration, acrocyanosis, and gangrene
- Mixed type cryoglobulinaemia — presents with intermittent palpable purpura (lasting 3–10 days); other signs include Raynaud phenomenon, psoriasis, cutaneous vasculitis, porphyria cutanea tarda, lichen planus, urticaria, and cold urticaria
Small vessel vasculitis
- Urticarial vasculitis — a leukocytoclastic vasculitis that affects about 5% of people with urticaria and is characterised by tender, burning, and painful papules or weals that persist for 24–72 hours
- Hypocomplementaemic urticarial vasculitis — this is a syndrome with chronic urticarial weals occurring for > 6 months, hypocomplementaemia, and leukocytoclastic vasculitis on biopsy
- Henöch–Schonlein purpura — this is an immune-complex mediated form of small vessel vasculitis that normally occurs in children, usually after a respiratory tract infection, and presents with purpura (leukocytoclastic vasculitis) and urticaria with local oedema; it can also cause intestinal vasculitis, intussusception (where one portion of an intestine protrudes into another), glomerulonephritis (inflammation of the kidneys), and joint symptoms (which are more common in adults than in children)
- Erythema elevatum diutinum — this is a chronic leukocytoclastic vasculitis that causes symmetrical red, violaceous, and yellow–brown papules, nodules, or plaques commonly on the extensor surfaces of the hands, knees, legs, and Achilles tendon
- Malignant atrophic papulosis (Degos disease) — this is a type of small vessel vasculopathy that presents with papules with a central white depression; the papules heal with a white scar.
Rare forms of small vessel vasculitis
Medium vessel vasculitis
Forms of medium vessel vasculitis and their associated skin signs include:
- Polyarteritis nodosa — this is a rare form of vasculitis involving small and medium-sized arteries of the dermis and subcutaneous tissue; skin signs (seen in 15% of cases) include red, blue, or violet subcutaneous nodules that become confluent and painful, livedo reticularis, leg ulcers, and postinflammatory hyperpigmentation
- Thromboangiitis obliterans (Buerger disease) — this is a form of vasculopathy due to thrombosis of small or medium vessels that is associated with smoking and is often asymmetrical and associated with cold climate or exercise; its skin signs are painful purple or blue fingers or toes (see blue toe syndrome) that may ulcerate or become gangrenous leading to amputation of a limb.
- Kawasaki disease — this is an acute multisystem vasculitis with fever,and systemic and cardiac manifestations; it is the most common cause of heart disease in children; its skin signs are polymorphous exanthem (90% of which are found on the trunk and proximal limbs), perineal eruption (macular or plaque-type erythema that desquamates within 48 hours); oedema and erythema of palms and soles; oral signs (including 'cherry' lips, dry and cracked 'strawberry' tongue with hypertrophied papillae, and dilated blood vessels), and periungual desquamation.
Medium-sized vessel vasculitis
Large vessel vasculitis
Forms of large vessel vasculitis and their associated skin signs include:
- Takayasu arteritis — this is a rare, systemic inflammatory large-vessel vasculitis usually involving the aorta and its branches and arteries going to the brain, limbs, heart, and kidneys that affects women aged 10–30 years; there are no associated skin signs.
- Giant cell arteritis (temporal arteritis) — this is an inflammatory condition mainly involving the blood vessels of the head and affects those 55 years of age or greater; its skin signs are cyanosis and pallor of extremities, scalp tenderness and sometimes, necrosis.
- Cogan syndrome — this is characterised by inflammation, predominantly of the aorta and its branches, and causes hearing loss, vertigo and eye symptoms; it has no associated skin signs.
Behçet disease
Behçet disease is a multisystem inflammatory disease affecting the skin, eyes, joints, and other systems. Its skin signs include:
- Recurrent oral aphthous ulcers> in 80% of cases<
- Genital ulcers in 64–88% of cases
- Erythema nodosum
- Pustules
- Superficial thrombophlebitis.